Cell Biology Researcher Response:
Dr. Patricia Inacio, PhD
Reprinted with permission by Multiple Sclerosis News Today
Blood infection with the yeast Candida albicans,a type of fungus, can reach the brain and trigger an immune response, a new mouse study shows. Although the fungus can be cleared within 10 days, it affects the spatial memory of mice.
These findings are the first evidence that a blood infection with a fungus may have a role in diseases linked with a deregulated immune response in the central nervous system, like multiple sclerosis (MS).
Microglia and amyloid precursor protein coordinate control of transient Candida cerebritis with memory deficits” was published in the journal Nature Communications.
Infections with the yeast Candida albicans have emerged as one of the leading blood infections in developed countries.
“An increasing number of clinical observations by us and other groups indicates that fungi are becoming a more common cause of upper airway allergic diseases such as asthma, as well as other conditions such as sepsis, a potentially life-threatening disease caused by the body’s response to an infection,” David B. Corry, MD, the study’s senior author, said in a press release. Corry is professor of immunology, allergy and rheumatology at Baylor College of Medicine in Houston, Texas.
Because the brain receives a large output of the blood pumped by the heart, it is susceptible to the effects of the blood-borneCandida albicans. For that to occur, however, the fungus has to cross the blood-brain barrier, a protective barrier that shields the central nervous system from the general blood circulation, including from pathogens that may damage the brain.
Interestingly, fungal infections that cause airway allergic diseases and sepsis (a generalized infection spread throughout the body) have been linked with an increased risk of dementia.
“These observations led us to investigate the possibility that fungus might produce a brain infection and, if so, the consequences of having that kind of infection,” said Corry, who also is a member of the Dan L Duncan Comprehensive Cancer Center.
Researchers at Baylor College of Medicine developed a mouse model with low-grade C. albicans infection. With this model, they prevented the infection from causing severe disease — as high-grade fungus infection is lethal to mice — but could study the fungus’ effects on brain function and the immune system.
The team tested doses ranging from 2,500 to 50,000 yeast cells, and set the dose of 25,000 viable cells delivered in a single injection to mice.
Using this animal model, researchers found that C. albicans fungi were able to cross the blood-brain barrier and reach the brain.
“We thought that yeast would not enter the brain, but it does,” Corry said.
Once in the brain, the infection induced a marked activation of microglia — immune cells of the central nervous system — including astrocytes, the most abundant glial cells.
“In the brain, the yeast triggered the activity of microglia, a resident type of immune cell,” Corry said, which “became very active ‘eating and digesting’ the yeast,” he added.
Moreover, activated microglia released pro-inflammatory signals — interleukin (IL)-1β, IL-6, and tumor necrosis factors (TNF) — and triggered the formation of fungal-induced glial granuloma (FIGG), a confined granule that trapped the yeast.
“They [microglia] also produced a number of molecules that mediated an inflammatory response leading to the capture of the yeasts inside a granule-type structure inside the brain. We called it fungus-induced glial granuloma, or FIGG,” Corry said.
To understand if the low-grade C. albicans infection had an effect on the brain’s function, researchers tested the performance of C. albicans-infected mice in well-established rodent behavior tests.
Compared to control mice (with no fungus infection), the animals infected with C. albicans showed impairments in a test that measured their spatial memory, called T-maze spontaneous alternation test.
Moreover, as the infection was largely cleared by day 10, so did the impaired memory. However, microglia cells remained in an active state, and FIGG persisted until at least day 21.
Overall, these findings highlight how a blood infection with a fungus can reach the brain and establish a successful infection. Moreover, once in the brain, the fungus triggered an immune response and, although the infection was resolved quickly, it triggered changes in certain functions within the brain, which supports a potential role for this type of infection in diseases like MS or Alzheimer’s.



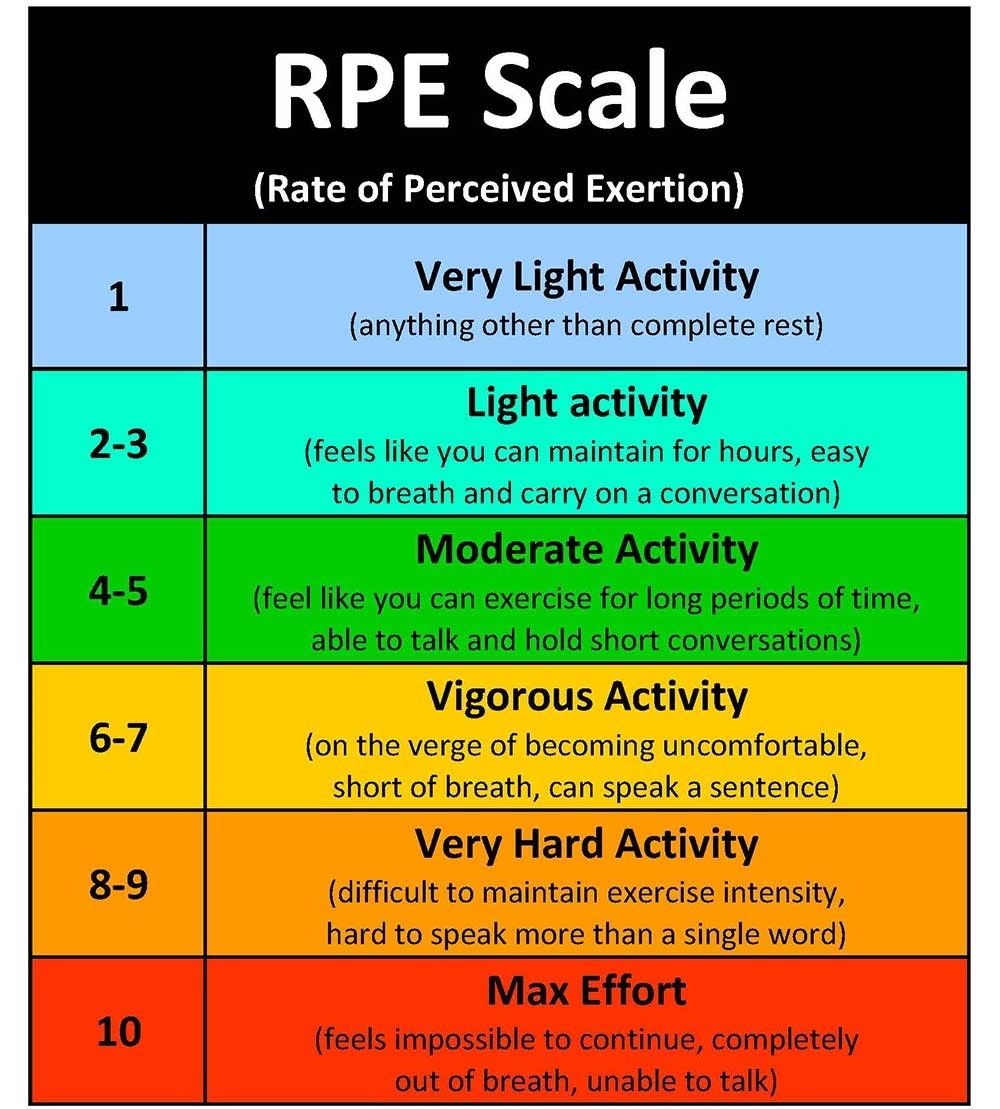
 The goal should be to adjust your exercise routine so that it gives you the best shot at reaching your sweet spot at the positive ends of these scales. Where you are today, this week, this month, may be different in the future. As your reality changes, you may need to change your exercise routine. You should always start this process by asking yourself, “What will keep/get me moving toward the positive end of these scales?”
The goal should be to adjust your exercise routine so that it gives you the best shot at reaching your sweet spot at the positive ends of these scales. Where you are today, this week, this month, may be different in the future. As your reality changes, you may need to change your exercise routine. You should always start this process by asking yourself, “What will keep/get me moving toward the positive end of these scales?”