DOUBLE Your Impact!
All donations will be matched dollar for dollar up to $50,000, but only until December 31! Your matched gift today will go even further to help people with MS live a better today and a brighter tomorrow.
Close
Frequently Asked Questions
Diet, Exercise & Healthy Behaviors
Psychologist Response
Roz Kalb, PhD
Senior Programs Consultant, Can Do MS
Thank you for the great question about adaptive pickleball. This sport is definitely catching on with people of all ages and ability levels. I’m not sure where you live, but in South Carolina, there is even an organization called www.adaptivepickleball.com that hosts pickleball games and events for people with disabilities. I would contact the YMCAs in your area to see if they have heard of any similar programs where you live. In the meantime, you can also find equipment that allows you to retrieve the pickleball without having to bend as far — including the EASY PICK pickle ball retriever and several other brands. You can search for them on Amazon by entering “adapted pickle ball retrievers.”
I hope you are able to find what you need to enjoy a game of pickleball!
Physical Therapist Response:
Mandy Rohrig, DPT
Senior Programs Consultant
Hello! Thank you for submitting your question to Ask the Can Do Team. I am sorry you experience this discomfort after activities. What you are experiencing could be related to MS fatigue, weakness caused by nerve fatigue, and spasticity; it is also possible it could be a combination of these challenges.
Spasticity can cause feelings of heaviness, pain, stiffness, or tightness. Consulting with a physical therapist or an occupational therapist who understands MS could further help to problem solve the precise cause(s) and more importantly strategies, such as stretching or tools, to help manage them.
In the meantime, here are a few strategies to consider:
Check out the resources on CDMS website specifically related to spasticity, fatigue, and ADLs, for additional information. Good luck!
Nurse Practitioner Response:
Kathy Costello, ARNP
Vice President of Programs, Can Do MS
Thank you for your question, and I am sorry to hear that you are having a cold sensation and discoloration in your feet. Some people with MS do experience a cold sensation and discoloration in the lower extremities, particularly the feet. Often this is seen when there is compromised lower extremity mobility. Having said that, it is important to have the signs and symptoms thoroughly assessed, as other conditions including vascular conditions, can also cause coldness and discoloration. If you have not already, I recommend that you let your PCP or your MS neurologist know about the symptoms you have been experiencing.
Psychologist Response:
Roz Kalb, PhD
Senior Programs Consultant, Can Do MS
Bladder and bowel symptoms are very common in MS. Damage caused by MS in the brain or spinal cord may interfere with nerve transmissions that control bowel and bladder function. These symptoms not only have a significant impact on your quality of life, but they can also impact other MS symptoms. For example, constipation, which is the most common bowel symptom in MS, can increase spasticity (stiffness) in your limbs and interfere with bladder function. Bladder symptoms can increase your risk of falls, disrupt your sleep, and make you more susceptible to bladder infections. And these infections, which can elevate your core body temperature, can make other MS symptoms like fatigue, weakness, pain feel worse. So, it’s very important that you report these symptoms to your MS provider and have a thorough evaluation.
As I mentioned, the most common bowel symptom is constipation. Adequate fluids, a diet high in fiber, a regular bowel schedule, and exercise are the best strategies for managing this symptom. Occasionally, loose stool may leak around a hardened, impacted stool. While this may appear like diarrhea, it is actually related to constipation and can be addressed by reducing the constipation. Diarrhea is uncommon in MS and is typically caused by another condition. Loss of bowel control can also occur in MS. The most effective strategy for managing bowel symptoms is to establish a regular bowel routine. I recommend that you read Bowel Problems – a publication from the National MS Society for a detailed description of bowel symptoms and the strategies used to manage them.
The most common bladder symptoms include a failure to store urine effectively, an inability to fully empty the bladder, or a combination of the two. I recommend that you read Urinary Dysfunction in MS, another booklet from the National MS Society for a description of the symptoms, the strategies used to diagnose them, and the treatments that are used. Managing these symptoms is important for your quality of life and your health, so don’t hesitate to discuss them with your provider.
Psychologist Response:
Roz Kalb, PhD
Senior Programs Consultant, Can Do MS
A review paper by Karpatkin and colleagues summarized what we know about the use of acupuncture in MS. Although this review was done several years ago, I’m not seeing any more recent studies:
“Use of acupuncture to treat multiple sclerosis (MS) is fairly common, but little literature exists which studies its effectiveness. The purpose of this paper is to review the literature on the use of acupuncture to treat MS. A literature search resulted in twelve peer-reviewed articles on the subject that examined the use of acupuncture to treat MS-related quality of life (QoL), fatigue, spasticity, and pain. The majority of the studies were poorly designed-without control, randomization, or blinding. Description of the subjects, interventions, and outcome measures as well as statistical analysis was often lacking or minimal. Although many of the studies suggested that acupuncture was successful in improving MS-related symptoms, lack of statistical rigor and poor study design make it difficult to draw any conclusions about the true effectiveness of this intervention in the MS population. Further studies with more rigorous designs and analysis are needed before accurate claims can be made as to the effectiveness of acupuncture in this population.”
Psychologist Response:
Roz Kalb, PhD
Senior Programs Consultant, Can Do MS
Thank you for your question. The answer isn’t a simple one because it involves your perception of weakness vs. your neurologist’s, as well as your definition of weakness vs. the doctor’s. When the neurologist measures weakness in your limbs, it’s an assessment that takes place at a specific point in time. The doctor is gauging the resistance in your limb at that moment. Is the weakness you feel present all the time or only after you have been using those parts of your body for a few minutes. In MS, there is something called “muscle fatigue,” which refers to a muscle that suddenly tires or runs out of gas after repeated use (while walking for example, or while engaging in extended activity with an arm or hand). After you stop the activity and give the muscle a chance to “catch its breath,” it feels OK again. If you feel weak all of the time, could it be MS fatigue as opposed to weakness that you are experiencing? Exertion fatigue in MS refers to the fact that daily activities often require more energy and effort for a person with MS than for someone else. This means that activities take more than the usual amount of energy because you have to exert more effort to do them with the result that feels more fatigued.
This is a long way of saying that a little more detective work may be required to figure out what’s going on. I would suggest that you consult with a physical therapist and/or an occupational therapist. They do different types of assessment than the neurologist typically does during a neurologic exam. They can actually measure strength more accurately and help you figure out what’s going on when you are engaged in activity. You can ask your neurologist for a referral or you can contact the National MS Society (1-800-344-4867) to ask for a referral to someone in your area. In the meantime, take note of when the feelings of weakness occur, what you’re doing at the time, and exactly what it feels like. This information will help the PT or OT assess what’s happening. I wish you the best. If you have additional questions, please don’t hesitate to get back to us.
The MyPlate Plan shows your food group targets – what and how much to eat within your calorie allowance. Your food plan is personalized, based on your:
They actually offer a few different tools that allow for folks who prefer to print the charts and also offer a phone app for those who prefer to keep track of things that way.
The charts are available to print (based on your nutrition needs which are roughly estimated by completing a short questionnaire here where it says, “Get My Plan”.
There is even guidance for shopping healthy on a budget via Shop Simple with My Plate.
And MyPlate is now available as an Alexa skill! Get MyPlate healthy eating tips on feeding babies and toddlers on your Amazon Alexa device OR on your smartphone or tablet via the free Amazon Alexa app.
One thing to keep in mind…the recommendations are based upon very basic health information and apply to generally healthy individuals. If you have any health issues that impact your nutrient intake (like kidney or liver disease) the recommendations may vary for you – or how you get the nutrients might be a bit different. But, with the input from your healthcare team and registered dietitian, these charts can still be very useful.
Read more about the tools that MY Plate offers here.
Psychologist Response:
Rosalind Kalb, PhD
Can Do MS Senior Programs Consultant
Thank you for your important question. It’s my hope that this response will help you as well as others who were reluctant to ask about erectile dysfunction (ED).
Erectile dysfunction is fairly common in men with MS. However, it’s important to remember that it occurs often in the general population as well. Common causes of ED include obesity, high blood pressure, high cholesterol, diabetes, smoking, stress and anxiety, a low testosterone level. Therefore, I urge you to discuss this with your primary care provider as well as your neurologist to confirm that the ED is related to MS and not to something else that needs your attention.
In MS, sexual dysfunction results from damage to nerve cells in the central nervous system that interfere with messages within and between the brain and spinal cord. Men report having difficulty getting and/or maintaining a satisfactory erection. Some also experience difficulty achieving an orgasm. Fortunately, men have several options for dealing with erectile problems. A urologist – a physician who specialized in the treatment of male and female urinary function and male sexual dysfunction – can help you determine which method(s) might work best for you.
Treatment options include:
Oral medications such as sildenafil (Viagra®), vardenafil (Levitra®), tadalafil (Cialis®), and avanafil (Stendra®) help by enhancing the effects of nitric oxide in your body. Nitric oxide is a naturally-occurring chemical that relaxes muscles in the penis to increase blood flow. This then allows you to get an erection when you are sexually stimulated. Oral medications work for many men with MS-related erectile problems, but not all. When the oral medications don’t work, there are other options to consider.
The injectable medication (papaverine) has been used to treat erectile dysfunction for several decades. It is a vasodilator that causes the blood vessels in the penis to expand, allowing for increased blood flow. While sexual stimulation is required when using one of the oral medications, a vasodilator like papaverine injected into the base of the penis produces an erection with or without sexual stimulation. In other words, it takes uncertainty or worry out of the situation. Although the thought of a penile injection may be very frightening, most men say that it is quite manageable – feeling like a flick of a towel. The base of the penis has fewer nerve-endings, which makes it a less painful spot.
A variety of mechanical options/implants are also available.
I would suggest that you look at the Intimacy and Sexuality brochure from the National MS Society for additional information. And if you have additional questions, be sure to get back to us. I also want to let you know that our November webinar will be on sex and intimacy as well.
Physical Therapist Response:
Mandy Rohrig, DPT
Can Do MS Senior Programs Consultant
Hi Deb! Thank you for your question and for reaching out to Ask the Can Do team.
Walking poles or trekking poles are lightweight “sticks” that offer balance during walking on even or uneven surfaces. Before purchasing this or any mobility aid, I would encourage you to make certain it is the most appropriate device for your needs. A physical therapist can help you trial and experience these devices both indoors and outdoors and help you make the choice of the mobility aid with the most appropriate fit and functional uses for your needs. You don’t want to waste your valuable time and financial resources with a device that doesn’t help you achieve your goals.
Before I share specifics, I want to briefly summarize the intended functional purposes for some of the more common mobility aids.
Considerations when exploring trekking/walking poles:
Remember, it is perfectly acceptable to explore a variety of devices and have a menu of options to choose from given the time, environment, and how your body is feeling. Good luck on your mobility aid exploration!
Psychologist Response:
Rosalind Kalb, PhD
Can Do MS Senior Programs Consultant
Thank you for this important question!
The simplest answer to your question is that the best diet for a person with MS is the same, healthy, balanced diet that is beneficial for everyone else. The diet should include:
This is closest to the Mediterranean Diet, which has been found to be beneficial for people with heart disease and type 2 diabetes. Both of these conditions are known to be common in people with MS and are also known to impact the course of MS. Although this diet has not specifically been found to help manage MS, it is among the most nutritionally complete dietary regimens and is also known to be anti-inflammatory.
Other diets – including the ketogenic and vegan diets — may have benefits for people with MS, but none has been adequately tested in well-controlled clinical trials. Research is ongoing that may help us answer these questions. Whatever diet you choose to follow, it’s important to make sure that you’re not depriving. Some of the more restrictive diets leave people feeling guilty, anxious, and frustrated when they find it difficult to stick with the plan. Eating should be both healthy and pleasurable. I would suggest that you consult with a Registered Dietitian to help you design an eating plan that best fits your needs, preferences, and budget.
Physical Therapist Response:
Mandy Rohrig, PT, DPT, MSCSC
Can Do MS Programs Consultant
Thank you for your question related to gauging how much you should push your exercise in the face of fatigue. This is an excellent question. Below are a few tips and strategies for someone with MS to consider when experiencing fatigue during exercise.
Some days are just fatiguing, and exercise is truly too much. Allow yourself constructive rest and recognize that your body needs to recharge. Good luck!
Psychologist Response:
Rosalind Kalb, PhD
Can Do MS Programs Consultant
Feelings of drowsiness can occur after eating, particularly after a big meal. Foods that contain tryptophan (which is used by the body to create the neurotransmitter serotonin) may contribute to feelings of drowsiness or sleepiness. These foods include turkey and high-protein foods such as spinach, soy, eggs, cheese, tofu, and fish. Fatigue after eating can also occur in people who have allergies to any of the foods they are eating. All of these contributors to post-meal drowsiness are related to the ways foods are digested in our bodies, which is unrelated to the causes of MS fatigue.
The cause of primary MS fatigue (also called lassitude) is still unknown. It generally occurs on a daily basis and often comes on suddenly. It may occur early in the morning, even after a restful night’s sleep. It tends to be aggravated by heat and humidity. Additional factors that contribute to feelings of fatigue in people with MS include: interrupted sleep and/or sleep disturbances such as sleep apnea; the extra exertion required to carry out daily activities, muscle fatigue caused by the overuse of individual muscles that tire from poor nerve conduction, among other things.
In summary, the fatigue people sometimes feel after eating is unrelated to the fatigue that occurs in MS.
Physical Therapist Response:
Mandy Rohrig, PT, DPT, MSCS
Can Do MS Programs Consultant
In terms of exercise and fatigue, any activity that raises your core body temperature even a tiny bit can cause a temporary flare-up in symptoms such as vision changes, brain fog, fatigue, and so on. Regulating your core body temperature can have a positive impact on your ability to participate in and recover from exercise. Using cooling products, such as vests, wraps, or ice packs among others, before you exercise for 10-15 minutes can lower your baseline core body temperature allowing you more leeway before you hit your threshold. Similarly, using cooling products both during and after exercise can help with your comfort during exercise and your recovery.
You may wonder, how do I know where my threshold is? How can you tell when you have crossed that “imaginary line?” First, I think it is important to recognize this “line” can move from one day to the next. So, what you are able to do on one day may be different than the previous. Fatigue, as you may know, can have not just an immediate impact after an activity, but also a cumulative impact, with excess activity one day triggering “exercise hangover” into the next.
Using a 0-10 scale, with 0 as no fatigue and 10 as maximal fatigue, can help you gauge how you are feeling and what may be the best exercise to do or not do. For example, if you are preparing to exercise, but you think your energy scale is at an 8/10, trying some gentle stretching may feel better than heavy weightlifting. Remember the 2-hour rule. If you don’t feel your energy or symptoms have returned to baseline within 2 hours after finishing the exercise you may have done too much and you may want to consider adjusting.
Please reach out to a physical or occupational therapist who understands MS to help you determine how to best manage your energy in a way that allows for optimal exercise and check out this related Can Do MS resource: https://www.cando-ms.org/multiple-sclerosis-programs/webinar-series/tired-of-being-tired-1. Good luck!
Dietitian Response:
Mona Bostick, RDN, LDN, MSCS
Can Do MS Programs Consultant
This is a great question!
A healthy lifestyle is a wonderful thing to share with your children. It involves a variety of health promoting behaviors including exercise and eating well. Because eating well does not mean something different because you are living with MS, everyone can enjoy the same meals together. Including children in the planning and preparation of meals can help them to feel involved and may contribute to their willingness to try new foods. Bonus, depending on the age of your children, it may take some of the work off you!
Meal planning and meal prep are tools to help you anticipate your meal-related needs for the week ahead and plan accordingly so that you arrive at mealtime without being overwhelmed. Planning involves determining how many meals will be required during the week and what those meals will be.
Meal prep involves getting you a few steps closer so that you are not starting from scratch every night. Maybe you invest a bit of time on the weekend to cook a roast (or other protein), chop veggies, tear lettuce for salads, or cook a pot of rice or other grain for use in meals later in the week. Prep could look very different depending on the meals you are planning. The idea is to invest a bit of time in advance to make sure you are closer to food on the table during the week.
Dietitian Response:
Mona Bostick, RDN, LDN, MSCS
Can Do MS Programs Consultant
In a word, no. For a number of reasons, three of which I will outline below:
1. Gut Health: While the gut is an exciting area of research, it is the early stages. Research is underway but not yet conclusive.
What We Know:
Research suggests that the microbial contents of the gut (Microbiome):
What We DON’T Know (yet)
In other words, the news is exciting and promising BUT, there is still a lot more to learn. And while the symptoms of food sensitivities/intolerances may manifest in GI symptoms, having a sensitivity or intolerance to a food does not mean your microbiome is unhealthy.
2. Allergies, sensitivities and intolerances
Like all allergies, food allergies generate an immune response when the problem food is consumed. Allergies can be reliably diagnosed via an IgE blood test, and a food challenge, done in a doctor’s office.
Allergies:
Food Intolerances/Sensitivities:
If you have a sensitivity or intolerance (say… lactose intolerance) you should avoid the problem food or be prepared for symptoms (Diarrhea? Bloating?). While the symptoms are uncomfortable, they are not life threatening and no permanent harm will be caused to the body.
There are a number of tests that are promoted to identify “food sensitivities,” though efficacy of those tests has been challenged. You can read more about that here.
3. Food sensitivity tests are very expensive ($500-$700.00 +) and are not covered by insurance.
They are often recommended by unconventional health providers to identify the root cause of a variety of symptoms including migraines, irritable bowel syndrome (IBS), hyperactivity, anxiety, irritability, arthritis, fatigue, muscle soreness, issues with balance and coordination, chronic infections, constipation, inflammatory bowel disease (Crohn’s, colitis), brain-fog, headaches, acne, eczema and weight gain.
If you are living with multiple sclerosis, you may recognize many of these symptoms and would love to get rid of them! But remember that MS (not a food sensitivity) is the likely culprit. Unconventional providers may recommend a test to identify your “problem” foods which they suggest are causing your symptoms. The results usually include a very long list of foods that the provider then recommends that you avoid. They then offer to sell you the supplements to replace nutrients that you are no longer getting from your food. You know, to prevent a deficiency!
Is there any harm in trying one of these tests? My answer to this is yes. Even if you are ok with the $500-$700 price tag, I would still steer you away from these tests and the diets, food rules, and supplements that always follow them. Removing a lot of foods from your eating pattern can begin to impact your mental health. It can create anxiety and fear around food. It will not impact multiple sclerosis at all. And according to the evidence, there will not be an improvement of the symptoms either.
I do not recommend any of these food sensitivity tests. They are a waste of money and mental energy.
Nurse Practitioner Response
Megan R. Weigel, DNP, ARNP-C, MSCN
Can Do MS Programs Consultant
This is certainly a timely question- as spring approaches, many people have trouble breathing because of seasonal allergies. In regard to MS and breathing problems, the answer to your questions are “Yes and yes.” If you have underlying lung disease and your oxygen levels are below normal, this may impact fatigue and endurance. MS can also cause breathing problems. Lesions can affect the diaphragm and other muscles of breathing. In turn, this can affect your ability to take deep and complete breaths. If you have had changes in mobility and muscle strength and a decrease in activity, this will affect your endurance. This means that activities that used to be easy may cause an increased heart rate and respiratory rate. MS is also associated with certain types of sleep apnea.
The National MS Society has an website dedicated to Breathing Problems that you might find helpful.
Occupational Therapist Response:
Stephanie Singleton, OTD, OTR/L
Can Do MS Programs Consultant
There are many pieces of adaptive equipment that can allow you to continue golfing. If you have issues with balance, there is the Solo Rider by Regal Research & MFG. Co which is a golf cart where the seat swings out to the side and assists the golfer with positioning while they swing the club. If hand strength is a concern, there’s a golf glove that assists with keeping a good grip on the club called a Stabilizer Glove. There is also a device that fits onto the end of the putter that prevents you from having to bend over to retrieve your ball after putting called the Nickel Putter Golf Ball Pick-Up.
Additionally, there is a device called the EZ-Tee that allows you to set the tee and ball without having to bend over. You could even check out a swing-less golf club called the PowerGolf Club by EGC. If you have foot drop, there are a variety of AFO’s that could be beneficial, including the TurboMed which attaches to the outside of any shoe that laces up and could be used with golf shoes. I hope that these items are helpful!
Physical Therapist Response:
Mandy Rohrig, PT, DPT, MSCS
Can Do MS Programs Consultant
Unfortunately, certain exercises or positions during exercise can be a trigger for muscle spasticity or muscle spasms. For example, sitting with just the ball of your foot touching the floor, and not the heel, could trigger clonus, or a bouncing of the foot/leg. For many, this is not only irritating but it could also lead to a calf muscle cramp or painful spasm. Another example may be a bridging exercise. With a bridge exercise, you are laying on your back with your knees bent and feet flat on the bed. You then lift your hips/buttocks off of the bed. This movement can be helpful with repositioning in bed or a useful exercise for core muscles and leg strengthening. Unfortunately, this too, can be an exercise that can trigger a painful hamstring muscle spasm.
Fortunately, you do not have to avoid these exercises or others that may trigger spasticity! Changes in the approach or position of the exercises as well as considering an alternative sequence of your overall exercise routine can be very helpful with minimizing or eliminating these painful spasms. Using the aforementioned examples, the calf spasm could be avoided by making certain heels are firmly on the ground whenever you are in a seated position. Or, you could also consider a calf stretch prior to assuming a seated position. If the hamstring spasms during bridges happens to you, try emphasizing pressure through the heels of your feet rather than the whole foot. Alternatively, adding a hamstring stretch prior to and perhaps after the bridging exercise can lessen the likelihood of a spasm.
Additionally, if muscle spasms and spasticity are frequently interfering with your functional mobility, I would strongly encourage you to talk with your medical team regarding potential medications that may be helpful. Talking in greater detail with your physical therapist about a stretching routine would also complement medication strategies well. Most importantly, remember exercise should not be painful. Please talk with your healthcare team if your exercise routine is causing pain. They can help you find activities that are beneficial to your health and mobility.
Neurologist Response
Randall T. Schapiro, MD, FAAN
Can Do MS Programs Consultant
Determining causes of death is not a simple process. This is especially important today during COVID when attributing death to the virus in individuals with other conditions. In a similar fashion the deaths reported from “multiple sclerosis” would not be in the same category as deaths in someone who had MS and was killed in an auto accident. The death rate attributed to MS itself is only a few percentage points greater than the general public’s death rate, but should not be significantly changed by falls, etc. I am sure there are some mistakes made in the numbers, here and there, but not enough to make a difference.
Nurse Practitioner Response
Megan R. Weigel, DNP, ARNP-C, MSCN
Can Do MS Programs Consultant
Absolutely not. In fact, melatonin has been studied as having a protective effect in one small study (https://hms.harvard.edu/news/melatonin-ms). In most people, melatonin is a safe sleep aid at low doses that may have protective antioxidant effects at higher doses. However, it can have side effects and also has many drug interactions. Melatonin is available over the counter, but you should always discuss new supplements with a healthcare provider before starting them.
Psychologist Response
Roz Kalb, PhD
Can Do MS Senior Programs Consultant
You are correct that most people are diagnosed with MS between the ages of 20-60; however, MS has also been diagnosed in very young children and older adults. It’s also true that people can develop MS at an early age but not experience symptoms until much later. I would suggest that you make a list of the symptoms or changes you are experiencing, as well as any previous symptoms or events that happened earlier in your life but disappeared. Discuss this list with your primary care provider and request a referral to a neurologist for further evaluation. Many different conditions can cause symptoms that are similar to MS, particular as one ages. It will be important to rule out any other possible causes of your symptoms so that you can get an accurate diagnosis and the best possible care, whatever the problem may be.
Given that you are in your 70’s, your primary care provider may say that MS is unlikely or impossible, so I would encourage you to advocate on your own behalf and request the referral to a specialist – to put your mind at rest and get an accurate diagnosis. You can also contact a National MS Society MS Navigator® at 1-800-344-4867 and ask for a referral to an MS specialist in your area. I wish you the best in finding an answer for your symptoms.
Can Do MS offers programs specifically on aging in MS that I would encourage you explore at www.cando-ms.org. This webinar has some great information on women’s health issues with MS.
Nurse Practitioner Response
Tracy Walker, FNP-C, WOCN
Can Do MS Programs Consultant
Although water is the best–technically any fluid other than alcohol or concentrated caffeine like expresso counts towards your total fluid amount.
HOWEVER- it is important to know that tea’s have other potential ingredients that can irritate the bladder other than just caffeine. So be sure you monitor your bladder after drinking the teas to see if they contribute to your symptoms. I also tell patients to drink water before and after drinking potential bladder irritants to hopefully dilute them when they hit the bladder and minimize urge and decrease leakage and urge incontinence.
Pharmacist Response
Lisa Aquillano, PharmD, BCPS, MSCS
Multiple Sclerosis Clinical Pharmacy Specialist, The Emory Clinic
The Multiple Sclerosis Association of America (MSAA) has a program to cover the copay or the cost of an MRI. The MRI Access Fund assists with the payment of brain and c-spine MRI scans for qualified individuals who have no medical insurance or cannot afford their insurance costs and require the exam to help determine a diagnosis of multiple sclerosis or evaluate current MS disease progression.
MSAA will refer you to an imaging center that is under contract with MSAA and will cover the cost of a brain MRI, c-spine MRI, or both. Or, they cover the cost of your medical insurance co-pay or co-insurance balance up to a maximum of $600 per MRI (cranial and/or c-spine). You will be responsible for costs exceeding $600 per MRI. MSAA will pay the billing facility directly. They will even provide payment for past MRIs, up to a maximum of $600 per MRI. To apply, visit www.mymsaa.org and click on “How MSAA Can Help”, then click “MRI Access Fund”. You can apply online by scrolling down to the large red buttons on the screen and choosing whether you are applying for a NEW MRI or a PAST MRI. Please note, before beginning the online application for a NEW MRI, you must have the MRI order/prescription from your doctor for a brain and/or c-spine MRI. You cannot complete the application unless you have this document scanned and ready to upload. If applying online for help with a PAST MRI, you will need to upload your MRI invoice. You may also download the application via the link on the website. Paper applications can be mailed or faxed to MSAA. For questions or to request a mailed copy of the application, call MSAA directly at 1-800-532-7667, ext. 120. You do have to meet income eligibility guidelines and comply with program requirements such as going to an MSAA-referred center. The direct link to the MRI Access Fund: https://mymsaa.org/msaa-help/mri/.
Infusion Administration Cost Help:
Medications that are administered in a medical setting (infusions) often include separate charges for the cost of the drug and the cost of the infusion center’s services. Many assistance programs will help with the cost of the drug but not with the cost of the administration. If you need help with an infusion administration costs and you are uninsured, it is recommended you explore the following options:
• The Assistance Fund’s Multiple Sclerosis Insurance, Travel, and Incidental Medical Expenses will consider assisting with the cost of infusion administration costs when funding is available. Check their funding status at https://enroll.tafcares.org/ or call 1-855-263-1772.
• Some pharmaceutical companies will consider helping with a portion of the administration costs. These are often separate programs than the programs that assist with the cost of the drug itself. Contact your pharmaceutical program to find out if they can help.
• MS Foundation Emergency Assistance grant provides full or partial financial assistance for urgent needs related to rent, utilities or medication. Please note: this is a one-time-use program. To learn more, call 1-888-MS Focus (888-673-6287), email support@msfocus.org, or start your application online at https://msfocus.org/Get-Help/MSF-Programs-Grants/Emergency-Assistance-Program.
• Make sure you’re using an infusion center that has lower costs. Hospital-based infusion centers can be much more costly than stand-alone infusion centers, although they might also offer charity care programs. Reach out to local providers to learn more about costs.
If you need additional help with locating resources, please contact the National Multiple Sclerosis Society by calling 1-800-344-4867, and ask to speak with a MS Navigator.
Can Do MS also provides additional resources on Access to Drugs and Healthcare, including my video on Increasing Your Reach.
Physical Therapist Response
Mandy Rohrig, PT, DPT
Can Do MS Senior Programs Consultant
Bioness(R) L300 (legacy/original model) and Bioness(R) L300 Go are functional electrical stimulation devices that are designed to help people who experience foot drop, including people with MS. Simply stated, a cuff around the lower leg stimulates the nerve to activate the muscle (tibialis anterior muscle) to pick up the foot with walking. The technology uses a sensor (heel switch in the L300 model and a gyroscope and accelerometer in the L300 Go) to know when to properly stimulate the muscle during the swing phase of walking. The Bioness may be fit and trialed under the guidance of an orthotist and/or physical therapist. When trialing the device, it is helpful to use it on a variety of surfaces and in a variety of environments to determine its effectiveness.
Your doctor and physical therapist can provide you with more information and help you determine if Bioness can help you.
Dietitian Response
Baldwin Sanders MS, RD, LDN
Can Do MS Programs Consultant
Inflammation is a very protective mechanism that your body uses to defend against infections and other injuries. Ever had a cut that turned red, made a scab and then healed? During this inflammatory process, the body:
1) Limits the blood flow
2) Provides a supply of chemicals like proteins, platelets, collagen to form a clot
3) Then makes a scab and starts healing!
But what happens when you have chronic, long-term infections? Chronic infections can lead to a multitude of problems. This can occur with or without symptoms and is common in gastrointestinal diseases, heart disease, insulin-resistance, cancer, as well as MS.
Lifestyle factors such as poor diet and stress can also lead to chronic inflammation. The standard American diet of highly processed foods, sugar, poor dietary fats, excess alcohol, and an abundance of calories can lead to chronic inflammation. Your body can benefit from stress reduction and an anti-inflammatory diet, such as the Mediterranean diet, which is also very tasty! It includes lots of fruits and vegetables that provide fiber, antioxidants, and phytochemicals that can protect your cells from damage.
A few other suggestions…
1) Include more fish and using olive or avocado oil, which provide Omega-3 fats that are anti-inflammatory fats.
2) Limited saturated fats- fried foods, cheese, fatty meats
3) Be aware of your sugars! Limiting sweets, sodas and processed foods are important in an anti-inflammatory diet.
Switching to an anti-inflammatory diet can provide you with multiple health benefits. Not only is this eating style delicious, but it is affordable, easy to follow, and a plan that you can follow for a lifetime.
Registered Dietitian Response
Mona Bostick, RDN, LDN
Can Do MS Programs Consultant
Thank you for the question. The Can Do MS Coronavirus and You webpage has some tips for grocery shopping and other tips for managing life during the current pandemic.
Now is the time to make sure your pantry is well stocked.
Because you may be preparing to stay home more than usual, it’s important to have healthful foods on hand. It also means shopping for food that will last for an extended period of time — about two weeks’ worth for those who are quarantined. I hope you won’t be holed up for too long, but just in case, here’s a list of foods to keep in mind when making your list.
Sanitize your shopping cart Use the wipes that grocery stores are providing at entry and using them to scrub down the handles of your cart.
What about produce? You can grab a plastic produce bag and put their hand inside and use that to pick up something like a head of lettuce. Then drop it into another bag and seal it up. Use the produce bag(s) kind of like a glove.
Skip the salad bar. Sneeze guards are not enough protection at this time.
Consider using your own shopping bags. These bags can be washed immediately after use and ready for the next visit. If you choose instead , to use disposable bags, check this out for more guidance.
Wash your hands, kitchen surfaces, and food. Wash your hands after returning home from the grocery. Wash your hands before and after you handle food. Wash countertops and utensils with hot soapy water between food items, especially raw meats, fish, and poultry. Wash fresh fruits and vegetables thoroughly before you eat or cook them. Clean the tops of cans before you open them. These are normal precautions, but this may be a good time for a refresher. Here is some more great information for food safety during this time.
What about take-out food? During this uncertain time, it is important to follow CDC guidelines along with all local regulations. It is also important to support small local businesses. Here is some great information about take-out and delivery foods.
What the heck should I cook? These times are a great reminder of how important it is to have back up plans, or strategies to use pantry foods for quick, easy and nourishing meals. Everyone has a few examples that they rely on but may be growing tired of the same old thing. To that end I’d like to poi t you in the direction of some inspiration! I am a big fan of Budget Bytes and she’s compiled a list of 15 pantry recipes. Smitten Kitchen’s blog is one of my favorite recipe resources. She’s also got a section for pantry recipes on her website. This is a great article from CookSmart that provided a wealth of information as well.
For additional information regarding MS Disease Modifying Medications and immunity the MS Society has provided guidance here.
Wash your hands, and be well!
Nurse Practitioner Response
Kathy Costello, MS, ANP-BC, MSCN
Vice President of Healthcare Access, National MS Society
According to the Red Cross, it is safe to donate blood.
Here is the link to their webpage on coronavirus and blood donation: https://www.redcrossblood.org/donate-blood/dlp/coronavirus–covid-19–and-blood-donation.htm
Nurse Practitioner Response
Kathy Costello, MS, ANP-BC, MSCN
Vice President of Healthcare Access, National MS Society
First, I am eternally grateful that nurses are providing care on the front line of the COVID crisis. There is a risk of coronavirus to every healthcare provider, but having MS does not increase that risk.
If the person is on a DMT, there is possible increased risk with some of the treatments – although this is not 100% certain. Please check the National MS Society website for more information about DMTs during the COVID crisis: https://www.nationalmssociety.org/What-you-need-to-know-about-Coronavirus-(COVID-19)/DMT-Guidelines-for-Coronavirus-(COVID-19)-and
Please continue to check the Can Do MS Coronavirus and Youwebsite for more resources.
Physical Therapist Response
Mandy Rohrig, PT, DPT – Senior Programs Consultant
Pregnancy, like Multiple Sclerosis, can be distinctly different for each mother. Similarly, each mother, can have distinctly different pregnancy experiences with each child. Therefore, I would highly encourage all mothers to discuss with their physician the appropriateness of exercise, prior to starting an exercise program. If given the “all clear” from the doctor, an individualized evaluation (even virtually, given the pandemic) by a physical therapist who specializes in women’s health may be especially helpful. A women’s health physical therapist can be found by checking out www.apta.org and searching for a women’s health PT. A mother could anticipate the PT discussing and providing instruction on exercises that optimize transverse abdominal muscle and oblique abdominal muscle strength, posture, gentle stretching, and low back and gluteal muscle strength, among others. The PT can help prioritize the exercises that are most appropriate and in the most optimal sequence for the mother’s situation.
Physical Therapist Response
Mandy Rohrig, PT, DPT – Senior Programs Consultant
I can appreciate the dilemma involving having another person coming into your home during the pandemic. While it is a wonderful opportunity to have her come to your home as it allows you to continue to participate in rehabilitation and exercise, you must also consider the amount of exposure she has had with the other clients and other people. While there is no definitive recommendation or standard of practice at this time, I would encourage you to have a thoughtful dialogue with your PT and perhaps other members of your healthcare team about the risk of her coming into you home versus the benefits and necessity of PT at this time. Can formal PT be “held” until the situation improves? Are there virtual PT opportunities? Can you continue with your current home exercise program at home and sustain your progress? I would also encourage you to talk with your PT about the organization’s cleaning strategies and personal/patient protection approaches given the pandemic. Clear and ongoing communication with your PT is key to developing a strategy that works best for you!
Registered Dietitian Response:
Mona Bostick, RDN, LDN
Can Do MS Programs Consultant
There is a lot of misinformation going around the internet regarding foods and supplements promoted to “boost” the immune system. The Novel Coronavirus-19 is new and evidence to support specific dietetic recommendations is not yet available in the scientific literature. It’s human nature to be looking for extra help to protect yourself from the coronavirus and COVID-19. But it is important to know that this is not how the immune system works. There really is no silver bullet.
There is no food, supplement or combination of both to heal or even treat the COVID-19 virus. Full stop. The very best way to support your immune system is by engaging in health promoting behaviors every day.
These habits include:
The best way to support your immune system everyday with your eating pattern is to include:
While limiting:
And avoiding entirely:
Building an eating pattern around these guidelines should provide adequate vitamins, minerals and phytonutrients for your immune system as well as the rest of your body.
Regarding supplements: If you are clinically deficient in a nutrient (as directed by your physician), or your diet is deficient in a nutrient (as may be the case if you are vegan- B12 -or a diet avoiding dairy which may require additional calcium then supplementing may be warranted. Again, under the guidance of your healthcare team. With any supplement, remember, they are not regulated, and more is not better.
The human body prefers to get nutrients from food. Nutrients from food come packaged in a healthy fiber and antioxidant filled “containers” which deliver nutrients in the manner our body finds easy to use. It is not necessary – and in fact may be harmful- to megadose vitamins and minerals. Fat soluble vitamins like A, D and E can become toxic at high levels.
Taking supplements will NOT impact the coronavirus. Learn more about supplements.
More Resources
Denise Nowack, RDN
Can Do MS Programs Consultant
Like most dietary choices, there are benefits and sacrifices with almond milk and cow’s milk. Comparing an 8oz glass of non-fat milk compared to 8oz of unsweetened almond milk, cow’s milk is higher in protein (8g vs 2g) and naturally richer in calcium. However, almond milk has about half the calories of nonfat milk. If you are concerned about carbohydrates, lactose creates about 12 times more carbs in cow’s milk. While almond milk is higher in fat (2g vs 0g), this is a healthy monounsaturated fat. Often almond milk is also fortified with added calcium and vitamin D.
So one is not “better” than the other. It truly is a matter of taste and choice.
In 2019, an international team of researchers published an article on Diet and Multiple Sclerosis. While they reconfirmed that “there is currently no scientific evidence supporting the use of specific diets in the management of MS,” they suggested an association with vitamin D and omega-3 fatty acid supplementation. Specifically, they suggested that removing cow’s milk may change the development and prevalence of MS, improve overall health, and lessen certain aggravating conditions associated with MS. Suggested replacements include rice milk, almond milk, and soy milk. There will certainly be more research on the impacts of almond milk and cow’s milk forthcoming.
For more information on food/beverage choices, including dairy products, here are some additional resources:
Can Do MS: Healthy Eating & Multiple Sclerosis
Can Do MS: Diet & Multiple Sclerosis
Neurologist Response
Ben Thrower, MD
Can Do MS Programs Consultant
The brain and spinal cord are composed of both grey matter and white matter. These term were used because they look grey and white in real life. Grey matter is the curvy outside part of our brain plus some deeper brain and spinal cord areas. It is mainly made up of neurons, but also contains axons (nerve fibers) and myelin (the insulation of the nerve fibers). White matter is made up of mainly the axons and myelin. In years past, it was felt that MS only attacked the white matter, but we now know that the grey matter is targeted as well. The classical view of MS as an inflammatory-demyelinating condition affecting white matter has recently been challenged by the results of advances in MRI studies that can also see grey matter.
The best thing we can do to protect grey and white matter is to have the person with MS on a therapy to prevent/slow relapses, new MRI lesions and progression of disability. Hopefully, research will give us options to actually repair damage and reverse disability in the future.
Physical Therapist Response
D. Michele Harrison, PT, ATRIC, ATP, CSMS
Can Do MS Programs Consultant
Depending on what activities you want to work on in the pool, it may be the best way to address fatigue and increase strength. In particular, you may want to work on walking with a heel-toe pattern. There are other exercises that can specifically be tailored to the ankle and foot in the pool.
The benefit is that it is cooler and you have the ability to do more with more range of motion in a pool. The fact that we work in a gravity environment for walking and functional activities, some of the work needs to be done on land. The pool depth could also be used to an advantage to increase ankle flexion and decrease the use of buoyancy and progress the activities as they can pick the foot up better. Neither the bike or swimming laps will increase the ankle strength for walking. I really don’t believe the elliptical would address that for waking either. Those activities are for cardio work and endurance rather than training weak ankle muscles, and there may be an increase of spasticity that could impede ankle function and lifting for walking.
I would recommend consulting a physical therapist that is experienced in MS and aquatic exercises.
Cell Biology Researcher Response:
Dr. Patricia Inacio, PhD
Reprinted with permission by Multiple Sclerosis News Today
Blood infection with the yeast Candida albicans,a type of fungus, can reach the brain and trigger an immune response, a new mouse study shows. Although the fungus can be cleared within 10 days, it affects the spatial memory of mice.
These findings are the first evidence that a blood infection with a fungus may have a role in diseases linked with a deregulated immune response in the central nervous system, like multiple sclerosis (MS).
Microglia and amyloid precursor protein coordinate control of transient Candida cerebritis with memory deficits” was published in the journal Nature Communications.
Infections with the yeast Candida albicans have emerged as one of the leading blood infections in developed countries.
“An increasing number of clinical observations by us and other groups indicates that fungi are becoming a more common cause of upper airway allergic diseases such as asthma, as well as other conditions such as sepsis, a potentially life-threatening disease caused by the body’s response to an infection,” David B. Corry, MD, the study’s senior author, said in a press release. Corry is professor of immunology, allergy and rheumatology at Baylor College of Medicine in Houston, Texas.
Because the brain receives a large output of the blood pumped by the heart, it is susceptible to the effects of the blood-borneCandida albicans. For that to occur, however, the fungus has to cross the blood-brain barrier, a protective barrier that shields the central nervous system from the general blood circulation, including from pathogens that may damage the brain.
Interestingly, fungal infections that cause airway allergic diseases and sepsis (a generalized infection spread throughout the body) have been linked with an increased risk of dementia.
“These observations led us to investigate the possibility that fungus might produce a brain infection and, if so, the consequences of having that kind of infection,” said Corry, who also is a member of the Dan L Duncan Comprehensive Cancer Center.
Researchers at Baylor College of Medicine developed a mouse model with low-grade C. albicans infection. With this model, they prevented the infection from causing severe disease — as high-grade fungus infection is lethal to mice — but could study the fungus’ effects on brain function and the immune system.
The team tested doses ranging from 2,500 to 50,000 yeast cells, and set the dose of 25,000 viable cells delivered in a single injection to mice.
Using this animal model, researchers found that C. albicans fungi were able to cross the blood-brain barrier and reach the brain.
“We thought that yeast would not enter the brain, but it does,” Corry said.
Once in the brain, the infection induced a marked activation of microglia — immune cells of the central nervous system — including astrocytes, the most abundant glial cells.
“In the brain, the yeast triggered the activity of microglia, a resident type of immune cell,” Corry said, which “became very active ‘eating and digesting’ the yeast,” he added.
Moreover, activated microglia released pro-inflammatory signals — interleukin (IL)-1β, IL-6, and tumor necrosis factors (TNF) — and triggered the formation of fungal-induced glial granuloma (FIGG), a confined granule that trapped the yeast.
“They [microglia] also produced a number of molecules that mediated an inflammatory response leading to the capture of the yeasts inside a granule-type structure inside the brain. We called it fungus-induced glial granuloma, or FIGG,” Corry said.
To understand if the low-grade C. albicans infection had an effect on the brain’s function, researchers tested the performance of C. albicans-infected mice in well-established rodent behavior tests.
Compared to control mice (with no fungus infection), the animals infected with C. albicans showed impairments in a test that measured their spatial memory, called T-maze spontaneous alternation test.
Moreover, as the infection was largely cleared by day 10, so did the impaired memory. However, microglia cells remained in an active state, and FIGG persisted until at least day 21.
Overall, these findings highlight how a blood infection with a fungus can reach the brain and establish a successful infection. Moreover, once in the brain, the fungus triggered an immune response and, although the infection was resolved quickly, it triggered changes in certain functions within the brain, which supports a potential role for this type of infection in diseases like MS or Alzheimer’s.
Nurse & Neurologist Response
Pat Kennedy, RN (Ret), CNP, MSCN & David Jones, MD
Can Do MS Programs Consultants
For many people, at some point in their disease course, typically after 10-15 years, relapses become less frequent or stop occurring completely, the disease progresses more consistently but not necessarily more rapidly, and changes in function become more pronounced. When that happens, the person is said to have transitioned to secondary progressive MS (SPMS). Approximately 15% of people are initially diagnosed with primary progressive MS (PPMS). This group tends to experience gradual changes in symptoms and function over time with very few or no defined relapses.
Our colleague and fellow Can Do MS Programs Consultant, Dr. Ben Thrower, explains the two disease courses as:
“Relapsing-Remitting MS: People with this type of MS experience clearly defined attacks of worsening neurologic function. These attacks, which are called relapses, flare-ups or exacerbations, are followed by partial or complete recovery periods (remissions), during which no disease progression occurs. About 85 percent of initial diagnoses are relapsing-remitting MS.
Secondary-Progressive MS: Following an initial period of relapsing-remitting MS, many people develop a secondary-progressive disease course in which the disease worsens more steadily, with or without occasional flare-ups, minor recoveries (remissions) or plateaus. Before disease-modifying medications became available, about 50 percent of people with relapsing-remitting MS developed this form of the disease within 10 years. Long-term data are not yet available to determine if treatment significantly delays this transition…
Because no two people have exactly the same experience with MS, the disease course may look very different from one person to another. And it may not always be clear to the physician, at least at first, which course a person is experiencing.”
We know that over time, people transition from a relapsing phase to a progressive phase, but it is difficult to know when this happens. MS goes from an inflammatory disease to more of a degenerative disease, and new lesions tend to occur less frequently in secondary progressive MS. Disability or symptoms tend to perhaps slowly become worse at different rates in different people. Everyone with MS is different, so the changes may be more rapid or may be very slow, and may create different physical or cognitive symptoms, depending on each individual person. There is still much to learn about progressive MS – from what it is and how to treat it.
It is important for people to have an understanding of what these terms mean so that if they receive the word that they have progressive MS, they can begin to think about how to plan for any changes that may occur.
To get a better understanding of your disease progression, you should consult with your neurologist and other healthcare team members. For more information on progressive MS, here are some additional resources:
Update Your Outlook On Progressive MS Can Do MS Article (with links to recommended resources from the National MS Society)
Update Your Outlook On Progressive MS Can Do MS Webinar
Progressive MS Can Do MS Webinar
Progressive MS Health & Wellness Resource Guide Can Do MS Article
Physical Therapist Response
Sue Kushner, PT, MS
Can Do MS Programs Consultant
Tai chi can offer wonderful benefits. There have not been a lot of studies specifically linking tai chi to MS, but there is certainly enough evidence to support that tai chi can lead to improvement in these areas:
-Improved balance (both in standardized tests and in functional balance measures)
– Improved Quality of Life (QOL)
– Decreased depression
– Decreased dizziness
– Improved postural control
In addition, a pilot study was just approved in April 2019 to measure the benefits of tai chi and mindful mediation on MS patients, specifically looking at the impact on physical balance and mental wellness. It will be exciting to see the results from this study!
For more information, I recommend contacting a physical therapist or other rehab professional trained in adaptive tai chi. The National MS Society offers a webpage and video about tai chi (there are several good adaptive tai chi videos on YouTube).
Dietitian Response
Mona Bostick, RDN, CSO, LDN
Can Do MS Programs Consultant
First, there is no research to suggest that a vegan diet will necessarily impact the course of MS, positively or negatively. One main benefit of a plant-based diet is that it tends to be rich in many nutrients. An analysis of National Health and Nutrition Examination Survey (NHANES) data found that the average intake of fiber; vitamins A, C, and E; thiamin; riboflavin; folate; calcium; and magnesium by those following vegetarian diets exceeded that of non-vegetarians, suggesting that vegetarian diets are nutrient dense and consistent with dietary guidelines.
However, just as with any set of dietary guidelines the first concern is with nutritional adequacy. In other words, are all of your unique nutritional requirements being met? Well-planned plant-based diets can be nutritionally adequate for people of all ages but there are some areas of concern including protein, omega-3 fatty acids, vitamins B12 and D, calcium, iron, zinc, and iodine. Read more here , here and here.
Can Do MS also has a number of great resources on the concerns and benefits of various diets, including this article by Dr. Pavan Bhargava
Dietitian Response
Mona Bostick, RDN, CSO, LDN
Can Do MS Programs Consultant
In a word, yes. Before I answer, I think it would be helpful to get a bit more specific about “inflammation”.
Inflammation is the body’s response to infection, injury or irritant. The body responds by sending an army of inflammatory cells to remove the stimulus and initiate the healing process.
Acute inflammation is a short-term response that can last minutes to days. The chemical mediators responsible for the vascular and cellular changes allow the flow of white blood cells and plasma to the site of injury (Think stumped toe). This can cause intense but temporary inflammation. Diet will not likely impact an acute inflammatory response.
However, prolonged (a.k.a. chronic) inflammation occurs when the cause of inflammation persists. This results in constant low levels of inflammation and can lead to serious health problems. These problems can include the buildup of fatty deposits in the inner lining of the arteries, which increases the risk for insulin resistance, stroke or heart attack.
Following a Mediterranean Style eating pattern along with other health promoting behaviors can positively impact chronic systemic inflammation.
Your efforts to manage inflammation through diet will be well complemented by addressing other health promoting behaviors, including:
Dietitian Response
Mona Bostick, RDN, CSO, LDN
Can Do MS Programs Consultant
In a word, yes!
The American Heart Association, The American Diabetes Association the Arthritis Foundation and the developers of the MIND Diet (and here) all encourage an eating pattern that is low in saturated fat.
A low saturated fat eating pattern promotes health and reduces risk for several chronic comorbid health conditions. This is important when living with MS because having a chronic comorbid health condition along with MS is associated with an increase in disability and a decrease in quality of life.
For more information, please check out my article and webinar on weight management and MS, which includes information on the impact of fats.
Nurse Practitioner Response
Cheryl Blaschuk, RN, FNP, MSN
Can Do MS Programs Consultant
Pelvic floor exercises, also known as kegel exercises, can strengthen the bladder muscles making it easier to hold urine for longer periods of times. They may help with urinary incontinence, which is a common symptom in MS. Because there are several types of kegel exercises, I recommend being evaluated by a physical therapist who specializes in pelvic floor rehabilitation. They can help create a specific exercise that will be both effective and safe for your physical abilities. The hardest thing is finding a pelvic floor therapist. Start with your neurologist, urologist, physical therapist, or a women’s health clinic. They should be able to refer you to a pelvic floor therapist, or someone else in the community who could make such a referral.
You should learn and practice exercises only after being evaluated. However, here is some more background information that you may be interested in:
“Bladder & Bowel Issues,” by Dr. Susan Kalota
“Bladder Issues,” by Pat Kennedy, RN
“Using Kegel Exercises to Manage Nuerogenic Bladder in MS,” by Dr. Revere Kinkle
“Pelvic Floor Disorders Are Common Among Patients With MS,” by Dr. Bruce Crawford
“7 Tips for Dealing With MS-Related Urinary Problems,” by Wendy Henderson
“MS research update – Pelvic floor training and electrical stimulation to treat bladder symptoms in women with MS,” by Multiple Sclerosis Trust
Physical Therapist Response
Courtney Capwell, DPT, MSCS
Can Do MS Programs Consultant
Foot drop is commonly caused by weakness in the dorsiflexors (the muscles that lift the toes away from the floor during walking) and plantarflexors (the opposing muscle group which point your toes when contracted). In order to improve foot drop, it is important to focus on strengthening both of these muscle groups. In addition, strengthening your lower extremity, specifically the hamstring muscle, is important for bending your knee appropriately, maintaining healthy posture, and performing weight-bearing activities safely and efficiently. Working with a physical therapist is a great way to initiate a full strengthening program. Physical therapists can provide appropriate exercises and guide you in correct performance.
I have put together some exercises on HEP2go that you may find helpful. You can access these exercises by visiting
www.my-exercise-code.com/index.php?uid=13d07a90a0a77272382c2c419fdf10cb and entering the code RP57HBB.
Before starting these exercises, consult with your healthcare team first to ensure you can perform them safely. Hopefully, they can start you on the path to managing these symptoms.
For more information, I would recommend this article and webinar on managing unique MS symptoms by fellow Can Do MS programs consultant and physical therapist Patty Bobryk.
Neurologist Response
Michelle Cameron, MD, PT, MCR
Can Do MS Programs Consultant
Despite its use by humans for thousands of years, the scientific study of cannabis and its components is still in its infancy. High-quality research remains limited. Based on existing evidence, cannabis products are probably effective for treating patient-reported symptoms of spasticity and pain. However, cannabis is probably not effective for MS-related tremor or urinary incontinence. People with MS should be aware of potential adverse effects of cannabis products, including new or worsening cognitive symptoms, psychosis, tolerance and dependence, as well as drug interactions.
The use of cannabis to treat MS symptoms remains controversial. Patients are encouraged to discuss these issues with their healthcare providers.
For more information, please view this webinar that I co-presented for Can Do MS on cannabinoids, as well as this article that I wrote. The National MS Society also has updated resources on Medical Marijuana and MS.
Physical Therapist Response
Kathy San Martino, PT, NCS, MSCS
Can Do MS Programs Consultant
Having a good exercise program is important for managing your MS and maintaining your mobility. A good comprehensive exercise program should include stretching exercises, strengthening exercises, balance, and aerobic exercises.
To avoid exacerbating fatigue issues, we tend to be conservative when creating an exercise program for individuals with MS. We try to prioritize what exercises are necessary and will try to choose exercises that will address several muscles at once. It is advisable that you see a physical therapist who can analyze your walking to assess what muscles need to be stretched and which ones need to be strengthened.
Let’s look at this example: In order to advance your leg with as little effort as possible, you must be able to bend the knee sufficiently when advancing the leg. If the muscles in the back of the thigh (hamstrings) are not strong enough, this can impede your ability to bend the knee. If the front of the thigh (quads) is spastic, it may be difficult to relax it to allow your knee to bend.
In other words, not only will the hamstring have to lift the weight of the lower leg, but it will also have to fight the quads which are trying to keep the knee straight. This quad spasticity can come in handy as it can keep your knee from collapsing as you’re standing on this leg.
In this scenario, it would be advisable to stretch the quads to diminish the spasticity (or prevent it from worsening) and strengthen the hamstrings. There are several versions of these exercises. A physical therapist could help you determine the most effective version for you and insure that you are performing the exercises accurately.
As I mentioned above, it is also important to perform exercises that help to improve your balance. If you can improve your balance, then this is one less issue that you are fighting when you walk. Sometimes balance exercises are as straightforward as working on your ability to shift your weight from one leg to the other. As walking becomes more laborious, it is easy to forget the mechanics of normal weight shifting.
It is also advisable that you see a physical therapist to determine if bracing and/or an assistive device would be beneficial. Basically, we’re looking for whatever devices are needed to make you walk more ‘normally’ When you are walking more ‘normally’, you will be walking with less energy, a decreased fall risk and decreased spasticity. Spasticity generally increases in proportion to the degree of challenge of an activity. An AFO can help you lift your toes. This often will help the rest of your leg advance easier and with less effort. An AFO will also relax any spasticity in the calf muscle. This in turn can help relax the spasticity in the rest of your leg. A Hip Flexion Assist Device can help you lift your leg and advance it with less effort which will also decrease the spasticity in the leg. An assistive device can assist with your balance and also decrease the challenge of walking (and decrease your spasticity).
An aerobic exercise program is important for heart health but also to improve your endurance. You probably notice that your walking is less than ideal when you are fatigued. With aerobic training, it will hopefully take more activity before you experience fatigue.
A PT can look at all these issues and help you put together the best approach to improve your walking.
Here are some additional resources with background information and ideas on exercise:
Nurse Practitioner Response
Megan R. Weigel, DNP, ARNP-C, MSCN
Can Do MS Programs Consultant
Over the past few years, some of the leading researchers in the field of MS have been trying to answer this very question, and so far the results are conflicting. In 2015, a study in JAMA Neurology reported that women who EXCLUSIVELY breastfed for at least 2 months had a lesser risk of relapse in the first 6 months following delivery than women who breast and formula fed, or women who did not breastfeed at all. This study found that, once the mother stopped breastfeeding, the relapse rates return to expected. Here is a summary of that study: https://www.medicalnewstoday.com/articles/298961.php
I tell patients that exclusively breastfeeding means that you cannot even think about formula or look at it in the grocery store! Regarding amenorrhea (absence of a menstrual period), exclusive breastfeeding causes a woman to stop menstruating to a certain point. It is the hormonal changes that are likely protective. This is a great review article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4757692/#B20
Bottom line is that the risks of postpartum relapses are much more related to the severity of your disease before pregnancy. If you were having frequent relapses even on disease modifying therapy, then you are more likely to relapse. If you have relapsing MS and your disease was quiet on disease modifying therapy prior to pregnancy, you are less likely to relapse. I recommend breastfeeding to women with controlled MS, and this often involves a long and honest talk about their desire and philosophy of child-rearing. It is very important to have a pregnancy and post-delivery plan. This includes discussing breastfeeding, restarting disease modifying therapy, and need (if any) for immediate postpartum therapies such as pulse steroids or IVIg. This is all based on the individual’s history of MS, and can’t be blanketed to a group.
For more information, the National MS Society has a website to News related to breastfeeding and MS: https://www.nationalmssociety.org/About-the-Society/News/Study-Finds-that-Breastfeeding-is-Associated-with
Nurse Practitioner Response
Tracy Walker, NP, WOC
Can Do MS Programs Consultant
So … It depends! A glycerin suppository may be enough. It works by lubricating and gently stimulating the lower GI tract to empty. However, a lot of folks need a stronger chemical stimulant such as Dulcolax suppositories. Those can be purchased over-the-counter, but sometimes they do not dissolve quickly enough to provide fast reliable action. There is another version called the magic bullet that is Dulcolax, but in a faster dissolving form. If your pharmacy does not carry those, you can purchase them online. If those don’t work some folks will try mini liquid enema’s such as enemeez. Every person is different, so you should ask your nurse, gastroenterologist, or other healthcare team members.
Nurse Practitioner Response
Tracy Walker, NP, WOC
Can Do MS Programs Consultant
Bowel issues with MS can be complicated because they can arise from several different issues. My approach to managing the problem usually involves the following:
Here are some additional resources that may be helpful:
“Bowel & Bladder Issues” Can Do MS Webinar
“Bowel Timing” Ask the Can Do Team Question
Nurse Practitioner Response
Denise Bruen, ANP-BC, MSN, MSCN
Can Do MS Programs Consultant
This is a great question and one that stumps many of my MS patients. New neurologic symptoms (numbness, tingling, weakness, vision loss, etc) that last longer than 24 hours continuously (and not in the setting of an infection) warrant a call to your Neurology office. This can indicate a relapse meaning a new area of inflammation in your central nervous system that should be evaluated and addressed.
Worsening symptoms over a short period of time (days to weeks) could indicate a pseudo-relapse. This means that there is not a new area of inflammation occurring, but rather something is taxing your body causing your old symptoms to be more obvious. This could be from an infection, lack of sleep, hot/humid temperatures, stress, or surgery (I have even seen this after prep for a colonoscopy).
If worsening symptoms occur over months or years this could mean progression of one’s MS and should be discussed with your neurology team.
Also remember that not every issue or symptom a MS patient has is necessarily directly related to MS.
Nurse Practitioner Response
Lynsey Lakin, FNP-C, MSCS
Can Do MS Programs Consultant
This is an interesting and timely question without a clear answer. These autoimmune conditions have been suggested to co-occur in a number of studies, suggesting that the two conditions share one or more components. One study observed patients with type 1 diabetes were at a more than 3-fold increased risk for development of MS. While there is an indication that there may be genetic factors that impact the prevalence of co-occurrence, some evidence suggests some environmental factors such as vitamin D deficiency may also contribute to the risk of developing both conditions. Another interesting factor is that there are ongoing studies around gut microbiota in both Type 1 diabetes and multiple sclerosis regarding how differences may contribute to any association of their development. This may potentially allude to reasons for co-occurrence or autoimmune conditions like Type 1 Diabetes and Multiple Sclerosis.
For more information, I suggest looking up these articles and be sure to ask your healthcare team.
Resources:
“The Dynamics of the Gut Microbiome in Multiple Sclerosis in Relation to Disease,” by Glenn Mowry; published in the Journal of Clinical Neurology in February 2018.
“Gut microbiota and Type 1 Diabetes,” by Yuing Hui Han et al; published in the International Journal of International Journal of Molecular Science in April 2018.
“Type 1 Diabetes and Multiple Sclerosis,” by Nete M. Nielsen et al; published in JAMA Neurology in 2006.
“The co-occurrence of multiple sclerosis and type 1 diabetes,” by P. Tetty et al; published in the Journal of Neurological Science in January 2015.
Physical Therapist Response
Jane Wetzel, DPT, PhD
Can Do Programs Consultant
While walking is certainly an excellent activity for weight loss, many individuals with MS have a problem with balance. Changing the TYPE of exercise can help tackle this problem. Research has shown you can burn calories most effectively if you use activities that use lots of lean mass… so both arms and legs should be moving. When we walk, we naturally incorporate arm swing. When your balance is challenging, you need to see if you can learn to walk with poles, which can be found inexpensively at many sports stores (Dick’s, REI, Cabela’s, etc.). The poles help keep your balance. You a can also burn lots of calories by using a NUSTEP or Aerodyne bike (see below)


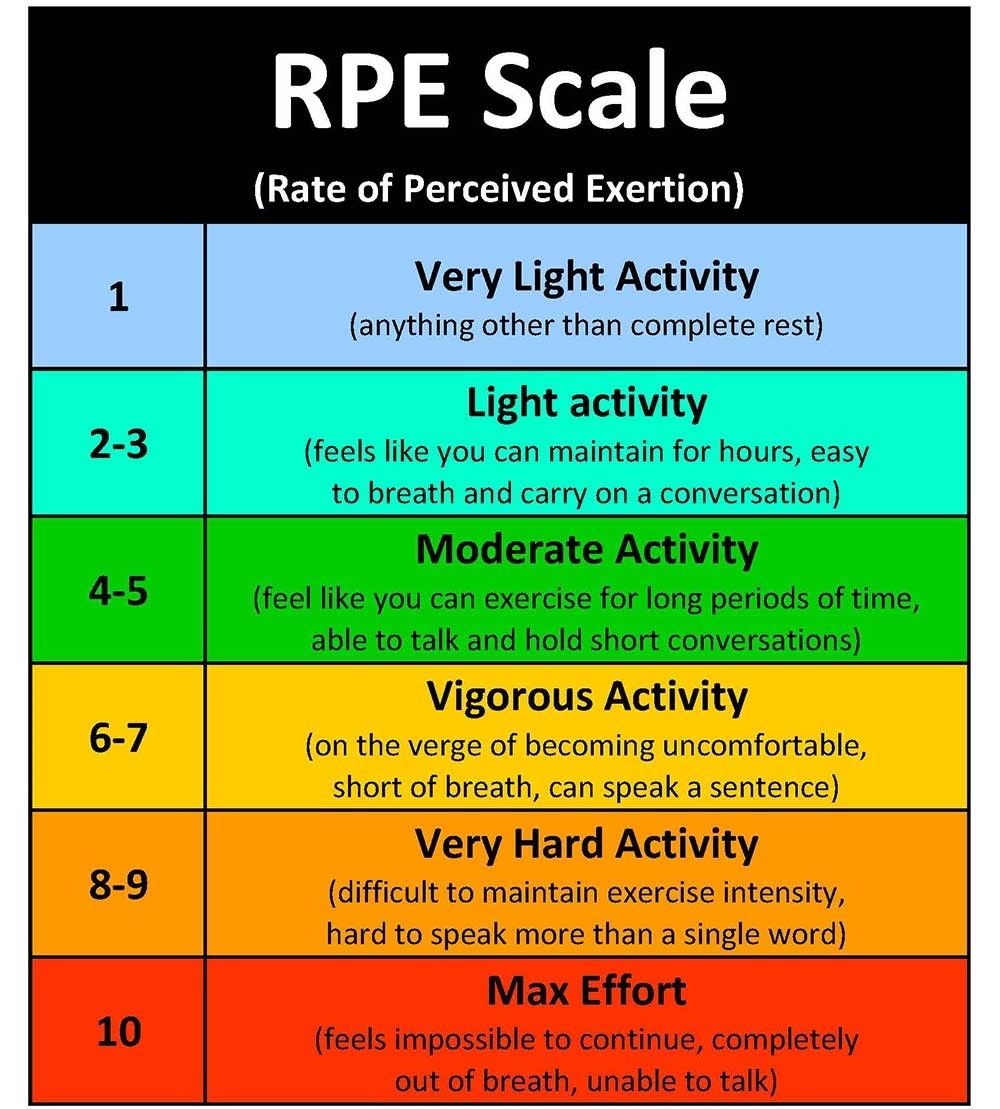
Once you figure out the types of safe exercises that work best for you (it is highly recommended that you consult a physical therapist or exercise physiologist), the next step is to figure out HOW LONG you should exercise. First, consider your RATE OF PERCEIVED EXERTION (RPE). The RPE scale (see below) is a way of measuring physical activity intensity level. Perceived exertion is how hard you feel like your body is working. You should focus on getting to a 4 or 5 on this scale (as PT can also help you understand what a 4 or 5 feels like for you). Then, start counting the number of minutes you can keep moving at a 4-5 rating. You need about 150 minutes a week.
Another great way to exercise while managing balance is to join a water aerobics class. These classes are often available at the local YMCA and have beginner groups. If you can handle deeper water, it will be easier to move without balance limitations. If you want to challenge yourself, move to shallow water. You might ask the YMCA if they can recommend a swim instructor with a background in modifying for special conditions and try a few individual lessons first.
Strength training can help with the coordination issues and also build lean mass. Try sitting in a chair and then standing, first with and then without armrests. Try first moving from a high seat…. Then lower the seat as you get better. Try and see if you can do five sit-to-stands in under 12 seconds…. Or count how many you can do in 30 seconds. Also work on lifting weights (which can be as simple as a can of beans) and strengthen the key muscles for stability – Calf muscles, Quadriceps, Hamstrings and Buttocks.
Also, remember that losing weight also has a lot to do with what you eat. A nutritionist or dietitian can help you develop a diet and plan of action. Can Do MS and the National MS Society offer a variety of programs and resources on healthy food choices that can help with weight management.
Losing weight is very challenging. Your team can also help you set reasonable goals, which are very important to implement sustainable behavior change that leads to positive and long-lasting outcomes. Set a reward for yourself- a movie, massage, etc.- then write down the food you eat the activity you do. Once you accomplish your goal, reward yourself! Then, set another reasonable goal.
There are many other resources on Can Do MS that can hopefully provide with more helpful information, including:
Weight Management and Nutrition Webinar
Exercise Physiologist Response
Alex Ng, PhD, FACSM
Can Do MS Programs Consultant
Thank you for this great question, and yes you heard correctly! Research in recreational ballroom and salsa dance for persons with MS has been published or presented recently that shows beneficial effects of partnered dance for persons with MS. (Because you mentioned foxtrot, I am assuming you are asking about partnered dance.) Benefits of regular social dance include improved endurance, balance, gait, self-reported quality of life, and cognition. As a bonus, dance is also a fun form of physical activity that can help persons with MS meet their exercise or physical activity goals. In the case of partnered social dance, your partner can act as a balance aid, allowing for activity that might not otherwise be safe.
There is no guarantee that regular dancing will increase the tempo of music you could dance to, but it might, and it could also improve your endurance or how long you can dance. If you are comfortable with a slow foxtrot, then you might also try a slow rumba or even a waltz. All these dances are danced in closed position which might be best if you are concerned about balance. In the case of waltz, instead of a box step you could modify the step pattern to a simpler country western style; in other words, you could ditch the box step in favor of a linear progression. The beauty of partnered social dance is that you can fit the dance type or music tempo to your ability. To summarize, there is no fundamental reason not to enjoy dance again if you are living with MS. You may need to experiment to find what works best for you, but once you dial it in, you may discover both physical and emotional benefits.
Here is a copy of a presentation I facilitated on dancing and MS. Your healthcare team, particularly a physical therapist, will also be a great resource to learn more about exploring dance moves that will be safe and beneficial for you. Your local chapter of the National MS Society may also connect you to local instructors who specialize in adaptive dancing.
Veterans Affairs Response
Angela Y. Young, Director of Education & Training
Multiple Sclerosis Center of Excellence – East
The Veterans Affairs Multiple Sclerosis Centers of Excellence (MSCoE) provide a wide range of life-long health care services to Veterans with MS. All enrolled Veterans have access to VA’s comprehensive medical benefits, but certain benefits will vary from person to person, depending on each Veteran’s unique eligibility status. The list below identifies some of the many services that may be available to you as a Veteran. For more information visit the Veterans Benefits Administration website at www.benefits.va.gov or www.vets.gov, or talk to a member of your VA health care team.
Through a collaborative integration of clinical care, education, research and informatics, MSCoE is improving health care services for Veterans with MS. For additional information, visit www.va.gov/ms.
Certified Therapeutic Recreation Specialist Response
Gus LaZear, MBA, CTRS
For Can Do MS, this is a very special topic because Jimmie Heuga believed very strongly in the importance of staying fit through sports, which can be modified around what you CAN DO. Here is a video of a Can Do MS adaptive golf experience. While your father may feel that he can’t play golf the way he used to, MS does not need to define his ability to continue playing the game he loves. A great example is Alice Plain, who also thought she had to give up golf after she was diagnosed with MS. Not only was she able to adapt, Alice became the PGA Director of Golf at Vail.
I am excited to hear that you are interested in learning about adaptive golf and getting active with your dad! First, I would find a local course that has an adaptive cart – such as a Solo Rider. You can learn more about what this is at http://www.solorider.com/. At my rehab facility in Phoenix, we have a unit called the Stand Up and Play paragolfer. Both work great, but they may not be for everyone. Some just need a regular cart and additional time.
To help determine what adaptations he may need, I would start by contacting your local office of the National MS Society. Society-sponsored adaptive golf experiences are becoming more popular across the country. They can also direct you to local organizations, such as Fore Hope, who have professionals dedicated to helping golfers adapt their game. Play Golf America, sponsored by The Professional Golfers’ Association of America (PGA), includes helpful information and resources, including an online search tool to locate PGA professionals with experience providing instruction to people living with disabilities.
Once you have determined your father’s needs and the right equipment for success (which are becoming more common and standard in the industry), it’s time to make sure YOU understand what you need to adapt, if necessary. As when you started golfing, it is important to go to the driving range, chipping and putting greens to learn or relearn basic golfing skills. Also, don’t feel rushed when playing golf, let others play through, and go at YOUR own pace. Maybe start with a par 3 course and grow into the back nine at your favorite course. With MS, understanding your environment and how it impacts you is the key to success. Start small and go from there.
Nurse Practitioner Response
Gail Hartley, MSN, NP, MSCN
Can Do MS Programs Consultant
Thank you for this important question. In short, MS does not discriminate on age. About 25% of people with MS are 65 and older, and they are certainly susceptible to symptoms and relapses. Although it has been reported that only 5% of MS patients develop new symptoms after age 50, this is due, in large part, because older individuals mistakenly believe their symptoms are related to the typical changes with aging, and, therefore, are less likely to see an MS care provider.
It is important not to jump to a conclusion and say that “an attack” is or is not related to MS, aging, or some other condition. Check-in with your health care provider! A careful assessment of your symptoms and appropriate medical tests are essential to making an accurate diagnosis and treatment plan. Then, focus on wellness. Take control of the things that you can do to stay healthy like eating a balanced diet, exercising regularly according to your ability, getting adequate sleep, and keeping a positive attitude.
Beware of what you read on the internet! There are some false claims on the internet that MS can “run it’s course.” According to Dr. Patrick Parcells, there is no research to suggest that “MS just does not progress beyond certain age ranges…some patients do continue to have slow, gradual progression.” Here is a recent article from the Cleveland Clinic that you might finding interesting. While it is possible that MS may “run its course,” damage to the central nervous system cannot be undone, so it is important to consult with your healthcare team as early as possible.
For more information, read this article on aging with MS that I co-wrote with psychologist Terri Di Lorenzo, and watch this Can Do MS webinar. This is also a good presentation by MS World and an article from Everyday Health.
Nurse Practitioner Response
Stephanie Buxhoeveden, MSCN, MSN, FNP-BC
Can Do MS Programs Consultant
A new shingles vaccine, Shingrix, is now available and is recommended over the older vaccine (Zostavax). Shingrix is a non-live vaccine, which is given in two doses. In general, it is recommended for anyone over the age of 50 regardless of whether you have had shingles in the past.
Shingrix has not been studied in people with MS, but in general non-live vaccines are recommended and often encouraged. Your doctor may have more specific recommendations depending on your MS therapy, so always check with your neurology team first.
Physical Therapist Response
Sue Kushner, MS, PT
Can Do Multiple Sclerosis Programs Consultant
Pain and stiffness are very common symptoms in MS. To find effective solutions, the first step is diagnosing the underlying cause from a doctor or nurse. Neuropathic pain, which is caused by damage to nerves, is much different than pain caused by mechanical problems, muscle imbalances, weakness, contractures, poor posture, orthopedic-based pain, etc.
In both of the cases you are describing, intervention by a physical therapist will be essential. They can recommend a stretching routine that will help the shortening of muscles and tendons that may be causing your pain. The National Multiple Sclerosis Society offers a great brochure on stretching for people with MS. Yoga has also been proven to be very helpful. Here is a brochure and webinar on how yoga can be an ally in managing pain and other MS symptoms. Both stretching and yoga can be adapted to any person’s mobility and activity-level.
A therapist can also evaluate your movement for overcompensation. Often, when a muscle or groups of muscles are very weak, the opposite (antagonist) muscles may take over, causing imbalances and pain. Strengthening exercises may correct these balances by helping nerves to fire properly. A physical or occupational therapist can also recommend bracing or other assistive devices, which may be beneficial for both issues. Finally, pain is often relieved when overall health improves. Regular, moderate exercise is essential to maintaining health and well-being for people with multiple sclerosis, and can cause a chain reaction to help your pain!
Specifically regarding your foot pain, this may be caused by cramping, spasticity, or improper gait. Massaging the foot and applying pressure to trigger (or pressure) points may also assist. Foot exercises with a small ball or a small foam cylindrical roller cans provide some relief. MS News Today and Everyday Health has some online at-home exercises. As always, I’d recommend asking your healthcare team which exercises will be the safest and most beneficial for you. Footwear is also essential in alleviating foot pain. A therapist and podiatrist can help you evaluate and adapt your footwear and foot functioning.
The pain when lying down may also be due to spasticity or orthopedic postural problems. Stretching and implementing proper positioning of hips, knees, shoulders, feet, pillow placement, and mattress choices may help with this.
Understanding the causes of pain in MS is also important. Here are some great resources for some background knowledge:
Pain and Depression in MS: Can Do Multiple Sclerosis Webinars
Understanding and Managing Your Spasticity: Can Do Multiple Sclerosis Webinars
Pain Management: Can Do Multiple Sclerosis Webinars
Pain: A Common and Complex Symptom: Can Do Multiple Sclerosis Library Article
Pain: National Multiple Sclerosis Society
Numbness of Tingling: National Multiple Sclerosis Society
Nurse Practitioner Response
Stephanie Buxhoeveden, MSCN, MSN, FNP-BC
Can Do MS Programs Consultant
Excellent question! Snoring is a common sign of sleep apnea, which, in turn, is very common in people with MS. Unfortunately, problems with sleep quantity and quality are particularly common among people with MS, affecting about 50% of the population. People with MS are also at greater risk for developing medical conditions such as sleep apnea. This is due to primary causes, e.g. lesion scars can make it harder for your brain to control your breathing your sleep, as well as secondary causes, namely weight gain frequently seen in MS patients due to fatigue and lack of activity
A 2012 study by the American Academy of Neurology suggested there is “a predisposition for obstructive sleep apnea and accompanying central apneas among patients with MS, particularly among those with brainstem involvement.” This predisposition to sleep apnea has both primary and secondary causes. Primary causes are directly related to the MS disease activity. For example, sleep can be affected when MS lesions occur in areas of the brain that are responsible for governing circadian rhythms (i.e., sleep-wake cycles within a 24-hour period) or the body’s essential hormonal and physiological processes, namely breathing. Disrupted breathing is a common cause of sleep apnea. According to the National MS Society, demyelination can also disrupt key neurotransmitters involved in sleep like hypocretin, dopamine, norepinephrine and melatonin, which can also result in sleep apnea.
Sleep problems can also occur as a consequence of the many co-occurring (co-morbid) symptoms that go along with MS, including fatigue, bladder/bowel problems, and issues related to mood and/or anxiety. Lifestyle behaviors such as exercise and environmental factors such as bedroom characteristics (e.g., temperature, light, etc.) can also influence sleep. Many medications present side affects that can also lead to sleep disturbances, including sleep apnea.
For more information on MS symptoms and medical side effects that can cause or worsen sleep dysfunction, please read this article that I wrote for Can Do MS, and brochure. Also check out the Multiple Sclerosis Condition Center. Finally, I highly suggest you consult with a doctor and sleep specialist to determine the cause and extent of your sleep apnea, as well as personalized management strategies.
Nurse Practitioner Response
Gail Hartley, MSN, NP, MSCN
Can Do MS Programs Consultant
Relapses, also known as exacerbations, occur unpredictably in MS. It can be difficult to recognize whether you are having a relapse (which is generally defined as new or worsening MS symptoms that last for more than 24 hours that are not associated with any other illness or infection), and even more difficult to determine why they are happening. According to the National MS Society, “there is no evidence that the stress of surgery will bring on an exacerbation of MS. Generally, in the absence of complications, people with MS who undergo surgery do not find that it impacts their neurological status.” There is also little evidence to suggest surgical anesthesia creates any more risk for persons with MS than in the general population. A recent study in Multiple Sclerosis also concluded that “surgery has not been found to be associated with exacerbations.”
The International Anesthesia Research Society agrees, although less definitively: “It has been speculated that general anesthesia and surgery may increase aggravation of MS. At present, there is no general consensus on this matter, and patients should therefore be informed of the potential for aggravated symptoms in the postoperative period.” These potentials include impaired autonomic functions, higher sensitivity to physical and emotional stress, and increased body temperature, all of which are common following surgery and can lead to disease exacerbations. Therefore, attention to physical and neurological therapy, emotional health, and temperature management are crucial following surgery.
With more advanced MS, anesthesia can aggravate certain muscle, neurological, and respiratory weaknesses, as well as increasing the likelihood for infection and fever- all of which can also lead to a greater risk of relapses. It is crucial that you consult with your healthcare team members, including your neurologist and physical therapist, about your particular circumstances.
While we cannot control when or how a relapse occurs, we can create a plan to rebound. In addition to talking with your healthcare team, please read this article and view this webinar, “Recognizing and Rebounding from an MS Relapse,” that I presented with fellow Can Do MS Programs Consultant, Sue Kushner.
Psychologist Response
Dr. Abbey Hughes, M.A., Ph.D.
Can Do MS Programs Consultant
Tremors, or uncontrolled movement/shaking, are common among people with MS and can significantly impact the quality of your sleep and your overall health. Tremors can occur in a variety of situations: during physical movement (e.g., when you are trying to reach for something like a pen or door handle); when you are supporting your body against gravity (e.g., when you are sitting or holding your arm stretched out); and during rest (e.g., while lying in bed). In addition to tremors, there are also two sleep-related movement disorders that are common in people with MS: restless legs syndrome (RLS) and periodic limb movement disorder (PLMD). In RLS, you may find the irresistible urge to move your legs, and this uncomfortable sensation tends to occur more in the evening hours and when you are trying to fall asleep. In PLMD, these movements occur during sleep, are uncontrollable, and the person is often unaware that these movements are happening.
For people with MS, there may be several causes of tremors or sleep-related movements. For example, lesions can cause damage to specific brain areas that control movement, resulting in tremors or uncontrolled movements. Second, some medications or combinations of medications can cause shakiness or tremor. It is important to make sure your neurologist or health care provider has a list of all of your current medications and dosages to rule out any medication side effects. Finally, there are some behaviors that can worsen tremors, even if they don’t cause directly cause the tremor. For example, excessive use of caffeine, alcohol, or nicotine/tobacco, lack of sleep, and even feeling highly stressed or anxious can worsen tremors.
As you can see, tremors and other sleep-related movements can be very complex. A neurologist who is trained in MS and/or sleep medicine can help determine what type of movements you are having, their cause, and potential treatments. This expert would be able to perform a physical exam and a sleep study to determine when the movements are occurring. As a psychologist, I cannot diagnose or determine the exact cause of your movements, but I can help patients learn relaxation and other strategies to cope with the discomfort that often comes with tremors. Reducing caffeine, nicotine, and alcohol use is often a good place to start, not only for tremors but for all of the other health benefits as well.
To find a sleep specialist near you, visit http://www.sleepeducation.org/find-a-facility and type in your zipcode.
For more information on sleep issues in MS, please read this article and watch this webinar I co-presented with fellow Can Do MS Programs Consultant Stephanie Buxhoeveden, MSCN, MSN, FNP-BC. Also, the National Sleep Foundation has some great resources on strategies to improve your sleep.
Physical Therapist Response
Mandy Rohrig, PT, DPT
Can Do MS Programs Consultant Coordinator
Cramps or spasms below the knee most commonly occur in the area of the calf muscle. I would encourage you to look for patterns in your activity to determine if that may be a contributing factor. Excessive walking, stair navigation, or exercise can trigger spasms later in the day and night…..or, maybe it is happening on days when you participate in too little activity. If you monitor your activity and there is no particular pattern, then I would talk with your doctor, nurse practitioner, or Physician’s Assistant to determine if there is a symptom, medication reaction, or even dehydration that may be contributing. A registered dietitian may also be able to find a nutritional deficit in your diet that could be leading to these cramps.
Furthermore, as a physical therapist, I have clients who experience spasms and cramps at night who find that a short stretching routine prior to bed can be helpful. A physical therapist can help you identify which muscle groups are tight, contributing to spams, and may benefit from more attention prior to bed. In the case of calf muscle spasms, a calf stretch in bed or prior to bed may be helpful for some. A physical therapist can provide a variety of positions to accomplish a calf stretch that would be most beneficial.
In MS, cramps can be caused by spasticity, which occurs when lesions damage nerve impulses that control muscle movement. There are a variety of exercises, medications, and medical interventions that can be used to treat spasticity, which, in turn, could help your cramps. I would recommend speaking with your healthcare team about this, as well. For more information, Can Do MS has published articles and webinars on spasticity management techniques.
I wish you relief from your cramps and a year of health, wellness, and happiness!
Dietitian Response
Mona Bostick, RDN, CSO, LDN
Can Do MS Programs Consultant
I would first determine if the knee pain is being caused by your muscles or bones (tibia, femur, or patella pain is more common than muscles around the knee). If the pain is indeed being caused by muscle cramps, certain mineral deficiencies could be contributing factors. I would look into deficiencies in three key minerals: potassium, magnesium, and calcium. Increasing food sources of these nutrients regularly may help to correct a deficiency. Here is a link to food sources of the mentioned nutrients (plus others, so scrolling will be required). I strongly discourage taking a mineral supplement without first speaking with their doctor as these supplements may interfere with medications.
Nurse Practitioner Response
Gail Hartley, MSN, NP, MSCN
Can Do MS Programs Consultant
Sneezing is an uncommon symptom in a neurological disease of any kind, including multiple sclerosis. Further, the actual mechanisms that cause sneezing are not well understood, but may include irritation of the trigeminal nerve endings that supply the nasal mucosa. Most of the time, chronic sneezing is related to inflammation of the nasal passages. Irritation can be caused by viruses or bacteria. Allergic triggers can include certain food, seasonal airborne pollens, dust, animal dander and weather changes. Certain medications, may also cause sneezing. Regardless of the cause, persistent sneezing should be thoroughly evaluated so that appropriate recommendations can be made.
Nurse Practitioner Response
Gail Hartley, MSN, NP, MSCN
Can Do MS Programs Consultant
A bowel retraining program can be very helpful for persons who have chronic constipation and irregular bowel movements, as well as for persons who have frequent loss of bowel control. Retraining your bowel involves trying to go to the bathroom at the same time every day to train your body to have regular and predictable bowel movements. It may take several weeks to establish a new routine, but it is possible with consistent effort and the help of a nurse and other healthcare team members.
Before starting a bowel program, discuss your current symptoms (ie constipation, incontinence) with your HCP. Review your current dietary habits–are you getting enough fiber in your diet? Are you drinking enough fluids? Are you getting any exercise? Are there medications that could be contributing to your symptoms?
The National MS Society has some great resources on managing bowel issues and can connect you with local experts who can help develop a retraining program. I’d also recommend this checklist of ways to regulate your system, as well as this article and webinar on bowel and bladder issues, all created by fellow Can Do MS Program Consultants. You can also access materials that we use at the 4-day CAN DO Program during the bowel and bladder workshops:
I hope you find these resources helpful and you can take steps to improve your bowel timing and overall quality of life.
Speech Language Pathologist Response
Pamela H. Miller, MA, CCC-SLP, MSCS
Can Do MS Programs Consultant
Multiple sclerosis can create weakness or incoordination of the tongue. This, in conjunction with other effects on your lips and soft palate, may lead to difficulty with speech and swallowing. This weakness can be caused by damaged neurons resulting from demyelination in regions of the brain connected to tongue activity, or it can be a side effect to some medications, particularly steroids. If you notice tingling or numbing on your tongue, changes to abilities to swallow or taste, or weakness in your tongue motions, you should talk to your neurologist and dentist. A speech language pathologist can also examine how you use your tongue and provide tips to manage these symptoms.
To gain a better understanding of the tongue’s muscular system, read this article by Sarah Gehke, MSN, RN, for Pacific Medical Training. The National MS Society and Everyday Health also have great resources about the impact MS can have on oral health. As the tongue plays an important role in swallowing, I would also recommend this Can Do MS article and webinar on safe swallowing tips from fellow Programs Consultant and speech language pathologist Janet DeClark, MA, CCC-SLP.
Neurologist Response
David Jones, MD
Can Do MS Programs Consultant
One of the most common questions that I am asked in my practice is in regard to stem cells. I suspect that the reason for this relates to differing goals between people with MS (wanting symptomatic and functional improvement) and that of the disease modifying therapies for MS, the current purpose of which is to reduce relapses, reduce new MRI lesions, and thereby delay disability. It is important to note that all stem cell manipulations for MS are still in research, with unproved efficacy and safety, and I would argue that having to pay money to participate in a research study is ethically questionable. Further, the long term safety of stem cell procedures is arguably incompletely defined in any disease state, especially one like MS in which the person may live for decades after diagnosis.
Much of the stem cell research in MS is with autologous hematopoietic stem cell transplantation (AHSCT, or “bone marrow transplant”), in which stem cells are mobilized from the bone marrow and then harvested from the blood. After this, high doses of chemotherapy are used to destroy the existing immune system, and the stem cells are reintroduced to “create a new immune system.” Several studies suggest this technique is very effective in MS efficacy, although there have been a few severe side effects (including death) in these studies; further, the goal of AHSCT is to stop progression of the disease and not necessarily to reverse pre-existing disability. Other stem cell research involve the use of mesenchymal stem cells, which may help modulate the immune systems attack of the nervous system and protect nerves from being irreversibly damaged. Studies with mesenchymal stem cells in MS are not as far along as those involving AHSCT.
The idea of using stem cells to repair pre-existing damage from MS still has some significant hurdles to overcome. Work is going on with remyelinating agents (including influencing resident stem cells to restore the myelin surrounding nerves); however, I would argue that the structure of myelin is more complex than typically recognized and involves more than just rewrapping a wire with electrical tape. Any attempts at remyelination requires that the wires of the nerves (axons) be intact, but unfortunately, much disability in MS is attributable to axonal loss. Restoring lost axons involves further issues, including ensuring that the correct connections are made between nerves and what they are supposed to control, which obviously is a difficult task. We spend a lifetime refining the connections between different parts of the brain as we learn new things and gain the ability to perform new tasks.
Other questions to consider with stem cells include how do the stem cells know where to go to correct the damage, how do they know how to not attempt to repair where there is no damage, and how do they turn off after the repair has been completed. There are complex signals that exist in a developing human to control these stem cells, and it is not entirely clear that these signals are as prevalent or in sync if exogenous stem cells are introduced into an adult. In summary, the idea of stem cell therapy for multiple sclerosis is very interesting and exciting, but there are still many questions in regard to the goals, efficacy, and safety (long and short term) of these techniques.
Nurse Practitioner Response
Gail Hartley, MSN, NP, MSCN
Can Do MS Programs Consultant
As flu seasons nears, this is a common question for people living with MS and concerned about injecting the inactivated virus from a flu shot. According to the National MS Society, the injectable flu vaccine has been extensively studied in persons with MS and is considered safe regardless of the disease modifying therapy one might be taking. However, it is recommended that persons taking Lemtrada or Ocrevus receive inactivated flu vaccine at least 6 week prior to their infusion. In addition, persons who are experiencing a serious relapse, or receiving steroids to treat a relapse, should defer vaccination for 4-6 weeks after the onset of the relapse.
Here are some other tips from the National MS Society:
For more information, watch this video by Dr. Mary Hughes.
Ultimately, all vaccinations present risks. However, for most people, the flu shot is safe and effective, particularly in light of the profound risks created by the flu virus (e.g. precipitation of MS exacerbations, complications on mobility, pneumonia). This is a great time to consult with your healthcare team to discuss your individual risks and benefits.
Physical Therapist Response
Mandy Rohrig, PT, DPT
Can Do MS Programs Consultant Coordinator
First, I applaud you for your initiative, investigative spirit, and interest to look “outside the box” at a variety of rehabilitation options. Many fine institutions, including Ohio State University, are taking significant steps to enhance clinical research and comprehensive care following spinal cord injury (SCI) to help individuals and their families re-enter into full community life. However, at this point, it is unclear the ramifications that this new relatively new research could have on MS rehabilitation. The American Congress of Rehabilitation Medicine and the Christopher Reeve Foundation have noted some similarities between interventions for people with SCI and MS. However, according to the National MS Society, rehabilitation for MS may be quite different because there is no “fixed deficit” like in SCI. In other words, the symptom profile of MS, the lesion burden on MRI, and the unpredictably fluctuating nature of individual autoimmune resources and the course of the MS, particularly following exacerbations, make it extremely challenging to determine whether a rehab strategy will or will not be successful.
Ultimately, I would encourage you to contact the rehab institution directly, in consultation with your healthcare team, for more information to determine if their services can and should be applied to your particular situation.
Urologist Response
Susan Kalota, MD
Can Do MS Programs Consultant
Incontinence is the inability to hold the normal amount of urine because of a spastic (overactive) bladder. In MS, this is happens when lesions block or delay transmission of nerve signals in areas of the central nervous system (CNS) that control the bladder and urinary sphincters. If you are experiencing some changes in your bladder function, you have a great deal of company. Probably 85% of people with MS will experience problems with bladder function at some time in their course of MS. It has personal and medical implications and is a symptom of MS that actually has a number of strategies to help. It is helpful to know a little about why this is such a commonly seen symptom. It is also helpful to know that bladder dysfunction can occur because of other problems as well so needs to be discussed with your family doctor, your neurologist or your gynecologist.
Bladders are told what to do by the brain and spinal cold. Peripheral nerves at the bladder send information to the spinal cord and brain. When brain, cord and bladder nerve s are working well, function is normal, but when MS causes lesions in the brain and cord, transmission of messages is slowed or interrupted causing you to experience symptoms. Why is this an issue? Symptoms can be inconvenient and uncomfortable and can intrude on your life style. You might have infections in either the bladder or kidneys or both. You can develop increased pressure in your kidneys causing major health issues. Problems can decrease your self esteem and can force you into isolation.
Bladder dysfunction falls into 3 categories. They are:
The symptoms for each can be similar so it is difficult to immediately know which type of problem you have. It is good to keep track of your symptoms and share them with your health care provider so that appropriate treatment can be initiated.
Storage problems occur when the brain is not able to allow the bladder to fill causing the bladder to empty frequently but completely. Symptoms include urgency, frequency, urge incontinence and few, if any, bladder infections.
Emptying dysfunction occurs when the messages to the bladder and its sphincters are slowed or absent so the bladder does not know it needs to empty or may not empty completely. Symptoms include frequency, urgency, urge incontinence, incontinence without urge, hesitancy, slow urine stream and history of bladder infections.
Combined dysfunction is a lack of coordination between the bladder muscle and the sphincters. This often traps urine in the bladder. Symptoms include urgency, hesitancy, dribbling, incontinence and infection.
If you experience any of these symptoms on a regular basis, talk with your provider. Depending on the symptoms, he or she might recommend a medication, a change in lifestyle, or a referral to an urologist.
So, bladder problems are an issue in MS but relief is available. Start keeping track and asking questions of your provider. Your good health and quality of life depend on it!
Click here to get even more great tips on this topic by viewing our archived webinar on Bladder Issues and MS.
Nurse Practitioner Response
Gail Hartley, MSN, NP, MSCN
Can Do MS Programs Consultant
Numbness, tingling, and burning sensations are commonly experienced by persons with MS. The severity of the symptoms can range from very mild to annoying to extremely painful. The degree of discomfort, or how much it interferes with your ability to function determines how aggressively this symptom needs to be treated. For some, no treatment at all is necessary. For others, pain that interferes with walking or other task may require medications.
Although I can’t provide specific advice, here are some general suggestions:
Note: If you notice significant changes in the intensity of your symptoms, or the symptoms have persisted longer than 24 hours, this could signal a relapse. Consult your neurologist to determine the appropriate treatment in this case.
There are a lot of great resources on tingling and numbness, including this video on the National MS Society website.
Occupational Therapist Response
Laura Kingston, OTR/L
Can Do MS Programs Consultant
I would first have you consider how you are going about your days before you “crash”. Do you pack your days with activity without any rest breaks or do you pace yourself throughout the day? If you have a daily “To Do” list, preplan a few 15-30 min breaks into your day. This will help you re-charge your battery BEFORE you begin to get fatigued. By doing this you will help prevent your body from hitting that wall of fatigue.
Think of your energy levels like a banking account… you need to decide how you are going to invest your energy (banking) and how you are going to expend your energy. You have to find ways to re-charge your battery in order to have energy to expend.
Some areas that can cause fatigue- aside from primary MS fatigue, which is caused by MS itself- are poor sleep, medication side effects, poor diet, high caffeine intakes (particularly in the afternoon which may disrupt sleep), uncontrolled spasticity, poor body mechanics, and increased core body temperature that is not managed well throughout the day. Also, inactivity is a major cause of “crashing.” Exercise and physical activity can actually give you energy that will help sustain you throughout the day.
Consider looking at any of these areas and make proper adjustments to help minimize your fatigue. An Occupational Therapist that specializes in MS can help you further analyze and provide specific fatigue management strategies for your lifestyle.
For some more tips on how to avoid the “crash,” please watch this webinar and read this article by Can Do MS. This is also a good article on fatigue management. Finally, Can Do MS’s in-person programs help you develop strategies to conserve energy and manage fatigue. I would highly suggest attending one if they are available in your area.
Physical Therapist Response
Mandy Rohrig, PT, DPT
Can Do MS Programs Consultant Coordinator
Thank you for this great question! Losing the ability to participate in the sports you love the way you are used to doing them can be very painful. However, the founder of Can Do MS, Jimmie Heuga, believed very strongly that you “can do” these great recreational activities with some adaptations.
First, I’m thrilled that you are passionate about the sports of kayaking. It’s a great way to build muscle strength in your arms, legs, back, shoulders, and torso. Men’s Journal recently named kayaking as one of the best workouts for heart health, decreasing fat and increasing lean muscle mass, as well as improving breathing and cardiovascular health. There is growing research into the benefits of kayaking, including this article in the Journal of Sports Science & Medicine Plus, it’s fun, serene, and provides great opportunities to explore!
Moreover, kayaking can be adapted to almost any physical ability. Single kayaks can be adapted to be powered by foot for people with arm weakness, or with deeper seat-pockets for those with trunk muscle weakness. Read this great article, “Outfitting A Kayak For Paddlers With Disability.”
There are also organizations across the country dedicated to providing instruction and opportunities for people to experience adaptive kayaking. I would recommend reaching out to the National MS Society, the MS Cure Fund, Disabled Sports USA, National Sports Center for the Disabled, and National Ability Center.
With the right equipment and support, you can absolutely continue to kayak. We hope you find the right fit for you!
Dietitian Response
Mona Bostick, RDN, CSO, LDN
Can Do MS Programs Consultant
This is a great question because there is an overwhelming information, particularly online, about supplements. Much of this information is marketing and advertising in nature rather than honest assessments based on research. Here are quick summaries on the supplements you have mentioned:
Ginkgo biloba: Recent research suggests that ginko biloba does not improve cognitive performance or disease course in people with multiple sclerosis. Please read my blog article on this here.
Ginseng: There is no evidence to suggest that ginseng offers any health benefits for folks with MS. Ginseng is an herbal stimulant with risks for side effects and medication interactions. It is a stimulant much like caffeine, but it also stimulates the immune system—which could, in theory, interfere with MS disease course or disease modifying therapies. Ginseng is also known to interfere with blood clotting and may interfere with medications like warfarin (Coumadin). Depending on the type of ginseng (Asian or Siberian), side effects vary from fatigue to stimulation and can impact sleep quality.
Take away: Save your money and avoid the risk…skip the ginseng and ginko biloba.
On the other hand, there is strong evidence to suggest that Vitamin D offers positive results, particularly in bone health. Deficiencies in Vitamin D is also linked with MS. Vitamin D supplementation is recommended, but there is not a universal dose as everyone absorbs Vitamin D differently. *It is important to have your doctor check your 25 hydroxyvitamin D levels and follow his/her recommendation about dosage. It may be trial and error that gets you to the appropriate dose for you but more is not better. I have also written about Vitamin D here.
As general advice, I recommend that you be cautious about supplements and be an informed consumer. Supplements are not regulated. So in my best Forest Gump voice… you never know what you’re gonna get. Seriously. Whenever supplements are warranted, I recommend the NatureMade brand (or other USP verified products). Always look for the USP label, which means they are third-party verified as to their contents. Another resource for this is consumerlab.com.
Finally, always speak with your doctor and/or pharmacist before taking any vitamins/minerals/ herbal supplements, as they can significantly impact other areas of your care. Make sure to include all supplements on any medication list.
Answer by Roz Kalb, Ph.D– Clinical Psychologist and Can Do MS Programs Consultant
As a mental health professional, I know that losing the ability to do something you enjoy is always a painful loss. Regardless of one’s disease course, MS can cause symptoms that gradually or suddenly interfere with home, work, and recreational activities. Watching others continue to do them with apparent ease only makes the loss more challenging to manage. The grieving process is not only normal and healthy, it is the first step towards finding satisfying and enjoyable alternatives that may become passions.
It is important not to compare your grieving to other people. The grieving process is unique to each individual — faster for some and slower for others. Some people need to grieve privately while others benefit from sharing the experience with others or with a counselor. Whatever your personal style, the important thing is to allow yourself this grieving time.
The next step is to allow yourself to consider options – looking at new ways to do the things you love and considering new activities that you might never have tried before. People who are forced to give up activities they love may try an activity they would never have considered in the past and discover a new interest. This may be “easier said than done.” My biggest recommendation is to utilize your support system and interdisciplinary health care team, who can work together to help you physically and emotionally. In particular, physical and occupational therapists are great resources to help you explore your options to stay active.
Answer by Mandy Rohrig, PT, DPT – Physical Therapist and Can Do MS Programs Consultant
As a physical therapist, I recommend a consultation with a rehabilitation professional – either a physical or occupational therapist – who understands MS. These professionals can help you understand your abilities, encourage exercises to optimize those abilities, and make adaptations to accommodate existing challenges.
If you excelled at cycling or did it competitively, you may feel disappointed in doing an adapted version of that sport. However, you may discover that you love the new challenge. The first step will be choosing the attitude in which you approach finding alternative activities that may need to be adapted to your physical abilities.
You will be happy to know that the world of cycling has expanded greatly to accommodate everyone! Three-wheel recumbents, arm or leg propulsion, or electric bicycles may be great options for you. I would recommend looking into electric bicycles because they allow you to pedal when able and use the electric feature when fatigued. Many areas have group classes and outings so you can feel the social connection that you enjoyed with bicycling.
Exploring other options for adaptive sports may be another strategy. Nationwide, there are organizations dedicated to providing adaptive sports and recreation, such as golfing, swimming, kayaking, and skiing can be adapted for individuals of varying ability levels.
We would encourage you to explore the following resources: www.disabledsportsusa.org and the National MS Society’s page about adaptive sports http://www.nationalmssociety.org/Living-Well-With-MS/Work-and-Home/Recreation-and-Travel/Finding-Another-Sport-to-Love.
A willingness to consider adaptations and viewing them as tools to participation is essential. Many people living MS and other conditions have faced similar challenges and have found ways to continue participating in sports they love. Perhaps speaking to or reading about others can inspire you. The founder of Can Do MS, Jimmie Heuga, epitomized this spirit of adaption and modification to allow him to continue enjoying skiing despite his disease progression. I would recommend reading Jimmie’s story: https://www.mscando.org/about-can-do-ms/our-mission/founder.
Thank you for your thoughtful post. We hope you find ways to be active and fulfilled.
Nurse Practitioner Response
Kathleen Healey, APRN, Ph.D.
Can Do MS Programs Consultant
Burning sensations are likely caused by spinal cord lesions, generally in the cervical or thoracic cord. The posterior part of the spinal cord is a sensory tract, and lesions here cause feelings and sensations (versus “motor tract lesions,” which impact body movement). Specifically, lesions on sensory tracts often cause burning, numbness, and tingling anywhere below the level of the lesion. Numbness and tingling in the legs and feet are common symptoms in multiple sclerosis. There are medications to treat this problem, as well as numerous other conservative measures that may improve symptoms.
Generally, the reason why people feel more tingling at night is that they are not preoccupied with activities during the day. Any symptom present when laying down to go to bed tends to be more obvious as there are no other “distractions”.
If this symptom has never been experienced before, it is important to notify your neurologist and other MS team members. Initial symptom that has never been experienced before may represent an active or new lesion in the spinal cord.
It is also important to know that for those diagnosed with multiple sclerosis, other diseases or problems (comorbidities) may occur. Although this symptom is likely due to MS, they could also represent a “peripheral neuropathy,” especially in MS patients who also have diabetes, thyroid dysfunction, lower levels of Vitamin B12, or other medical conditions. Notify your health care team as soon as these symptoms occur so they can help you sort out the potential causes and recommend appropriate management strategies.
Dietitian Response
Mona Bostick, RDN, CSO, LDN
Can Do Programs Consultant
While researchers are beginning to study the impact of Vitamin E on MS, there is no evidence that Vitamin E supplements offer specific benefit for people with MS. In fact, taking high doses of antioxidants like vitamin E may be detrimental for folks with MS. Large doses of vitamin E supplements (>400 IU) may also increase the risk of prostate cancer and bleeding. Vitamin E supplements can also negatively interact with anticoagulant medications such as warfarin (Coumadin), as well as chemotherapy medications.
The recommended dosage for Vitamin E for adults is 15 mg (22 IU), which is tough to get from a supplement since most supplements exceed these numbers by far. More is not better. With this in mind, I would recommend consulting a professional before taking any Vitamin E supplements. First and foremost, deficiencies in Vitamin E are rare. Secondly, food sources of vitamin E are plentiful and easy to include in your diet. Vitamin E rich foods include wheat germ oil, nuts, seeds, nut butters, vegetable oils, and spinach (cooked has more than raw).
Bottom line: skip the supplements and include vitamin E rich foods in your diet.
Physical Therapist Response
Kathy San Martino, PT, NCS, MSCS, CLT, ATP
Can Do MS Programs Consultant
First, address weakness in the anterior tibialis muscle (the primary muscle responsible for lifting your toes). In a sitting position, perform toe taps. The anterior tibialis muscle is located to the outside of the shin bone so you should note a muscle contraction here when performing toe taps. Be sure the foot is lifting up straight. In other words, neither the big toe nor the little toe should be leading.
Foot drop can also be caused by – or exacerbated by – a tight or spastic gastrocsoleus muscle ( the muscle in the back of the calf). >span class=”apple-converted-space”> seconds.
Lastly, it’s important to work on your motor control of the leg. In other words, even if you have the right amount of flexibility and strength in your ankle, it is necessary to develop the motor control to use the right muscle at the right time and the right amount. So now, take the time to practice walking. Slow down your speed enough to focus on picking up your toes when you lift your foot to step forward. Your foot should then hit the ground with your heel first. Gradually work on increasing your speed of walking while preventing foot drop with each step.
Sometimes an AFO/brace or electrical stimulation device is needed to control foot drop. Some people are worried about losing more control of the ankle by using a brace. The brace actually can control the spasticity in the calf muscle and prevent this muscle from developing a permanent contracture. The brace can be built to allow you to use whatever muscle control you do have in your ankle. Consult your health care team, particularly a physical therapist, to determine which brace or mobility device will best help you stay walking as normally as possible. This is important not only for safety, but also to maintain your endurance and the normal function of the rest of your leg.
Exercise Specialist Response
Marina Moldavskiy, BS
Can Do MS Programs Consultant
I’m sorry to hear about this new onset of spasticity. Please make sure to consult your neurologist if it is causing you pain or interfering with your physical function, activities of daily living, or sleep cycle.
To manage your spasticity and increase strength/range of motion, it is very important to incorporate a stretching regimen into your daily routine, even on days you are busy. While your hamstrings may be causing you the most trouble, it is also important to “give love” to all your muscle groups – hips, glutes, hamstrings and quads. The order and detailed instructions of these exercises will depend on your individual abilities and body dynamics. An exercise specialist or physical therapist can help you develop an individualized stretching program and put exercises in order that will be most beneficial to you.
To start you off, I compiled some strengthening and range of motion exercises that specifically addressing spasticity issues on www.my-exercise-code.com. To access these exercises, enter the following code: B7SC7LY. All of these exercises can be done at home, using a bed, chair, or tabletop surface to hold onto. Start easy and increase the time and repetitions for each exercise when you feel ready to progress.
Finally, you should consciously integrate elements of dynamic stretching, passive stretching, and static streching in your program:
A foam roller is also something great to invest in. Most come with a card that demonstrate the stretches you can do. You can find them on Amazon.com.
Stay consistent and do not give up! You can do this!
Answer by Mandy Rohrig, PT, DPT – Physical Therapist and Can Do MS Programs Consultant
Riding a recumbent bike may enable you to reach your fitness goals without increasing fatigue or exposing you to injuries from a loss of balance. In addition to being a fun activity that can be adapted to almost every ability, bicycling can help MS patients reduce stiffness/spasms and improve balance, gait, mobility, flexibility, and motor control. As you alluded to, you can continue to enjoy your passions with a little creativity and adaptation. For many people with MS, recumbent bicycles are a great solution!
According to Michele Turcotte, MS, RD, from the National Academy of Sports Medicine, “[t]he recumbent bike design allows you to comfortably distribute your weight over several square feet of the back and buttocks whereas on an upright bike, your body weight rests on only a few inches of the sit bones, feet and hands. For many riders, this positioning places stress on the wrists, depending upon how you sit, and can be uncomfortable. If ridden for more than 20 minutes, this discomfort may be intensified. If you’re riding a bike outside, recumbent bikes have an aerodynamic advantage. The reclined, legs-forward position of the rider’s body creates a smaller frontal profile, increasing efficiency and maximizing speed.” There have been other scholarly work identifying the benefits of recumbent bicycles, including this article by Regina Boyle Wheeler for Everyday Health.
However, Ms. Turcotte also points out that a recumbent bike may not be the ideal activity for everyone. An upright stationary bike may be more appropriate depending on your individual abilities and comforts. Arm bikes may also be a better solution for some, while others would be better suited to an eliptical machine. I would recommend consulting a physical therapist or personal trainer familiar with MS to determine which equipment will work best for you!
Finally, for some general tips on cycling, please read this article by former professional cyclist Tyler Hamilton. Tyler has been raising awareness about adaptive cycling for years and has partnered with Can Do MS on several programs. Read more about how Tyler is supporting MS Global. Perhaps you can get involved with this great international event that makes profound differences for people living with MS.
Answer by Mona Bostick, RDN, CSO, LDN – Registered Dietitian Nutritionist and Can Do MS Programs Consultant
Clinical studies suggest that flaxseed oil and other omega-3 fatty acids may be beneficial for a variety of conditions. However, there is no recommended dosage or regimen. With flaxseed oil, there are potential interactions to consider. It is best for any recommendations to come from a healthcare provider familiar with your needs and contraindications.
For more information on flaxseeds and other nutritional tips, check out this article by a fellow Can Do MS Programs Consultant, Aliza Ben-Zacharia, ANP, DNP, MS. Pharmacy Times also published an informative article on the potential benefits of flaxseed oil in MS.
Physical Therapist Response
Amanda Rohrig, PT, DPT
Physical Therapist and Can Do MS Programs Consultant
Thank you for your question! First, I must commend you on your amazing commitment to exercise and consistent physical activity! Wow! Way to go! I also commend your sensitivity and awareness to ensuring you participate in aerobic exercise, as it is an important component to a comprehensive exercise program. Furthermore, there continues to be a growing body of emerging research suggesting the value of aerobic exercise for people with MS for not only the health of our bodies, but also the health of our nervous systems (i.e. potentially slowing disease or influencing lesion burden).
Aerobic exercise, as I suspect you may know, involves increasing the activity of the heart and lungs. Aerobic literally means “requiring oxygen.” The recommended guidelines for people to achieve an aerobic exercise zone for the heart rate ranges from 60-85%. I generally recommend between 60-70% of the heart rate maximum. Heart rate maximum can be estimated by the following equation: 220-age=maximal heart rate. This number can then be multiplied by 60% and 70% for an estimate of your aerobic exercise zone. However, often it is helpful to use a 0-10 exertion scale versus heart rate, so you do not have to go to the trouble of measuring heart rate in the middle of exercise. So, you would reflect on how “hard you feel” yourself working; 0 equating to no effort and 10 is maximal effort. A good aerobic exercise effort would be 3-5/10 intensity. All that said, perhaps, you are actually working out at an aerobic intensity level.
Types of exercise that may be considered aerobic at the proper intensity would include (but certainly not limited to): walking, stationary biking, swimming (laps may be more effective for you), or rowing machines. If you find that overheating is a barrier to exercising at an aerobic intensity, then I would recommend potentially trying the pool, especially if the water is cold (NOT warm water pools). Other ways to keep your core temperature more moderate while you are exercising may include: 1) drink cold drinks while exercising 2) keep fans blowing directly on you throughout the workout 3) wear cooling products, such as cooling vests, wrist ice wraps, or ice packs around the neck/shoulders. 4) break-up your workout into two parts, allowing you the opportunity for your heat-related symptoms to subside, finishing the workout at a later time or once your symptoms are not as pronounced. Lastly, I would strongly encourage you to seek the individualized guidance from a PT who understands MS and can truly help you shape your exercise program to maximize your success. Good luck and happy exercising!
For more information on exercise, visit Can Do MS’s extensive library of webinars and articles, including this article on endurance and aerobic activity.
Also, please join me, along with dietitian Mona Bostick, at the upcoming Can Do MS webinar ,”Weight Management and Nutrition,” by registering here.
Answer by Mona Bostick, RDN, CSO, LDN – Registered Dietician Nutritionist
The simple answer to this question is no. Vitamin D is a fat-soluble vitamin and does not impact the absorption of (water soluble) vitamin C. In other words, both vitamins are important partners in a balanced diet, but they work independently and are processed differently. I would certainly discuss this balance with your health care team. High doses of vitamin D may be react adversely with other drugs. High amount of both vitamins have also been linked to increase risk for kidney stones. Unlike vitamin D, vitamin C is readily available in food and deficiencies are rare in developed countries; so supplementing is not commonly necessary. Talk to your doctor about your specific health and diet needs.
For more information on Vitamin D, read this response from Can Do MS Programs Consultants Baldwin Sanders, MS, LD, RDN and Barbara Giesser, MD, and this article by Pat Kennedy, RN, CNP, MSCN. To learn how vitamins fit into a balanced diet and their potential impacts on MS, read this article and view this webinar by Dr. Pavan Bhargava, MD. Finally, join me, along with physical therapist Mandy Rohrig, PT, DPT, at our upcoming webinar on nutrition and MS.
Adaptive Yoga Instructor
Founder of Bamboo Yoga Studio
Ann Richardson
I am so happy to hear you are interested in yoga. Unfortunately, there isn’t a database for MS yoga instructors. Yoga Heals Us has a nationwide list of adaptive yoga instructors at http://www.yogahealsus.com/gpage3.html. I would also check with your local MS centers, support groups, physical therapists, etc. The staff at Studio Bamboo can also direct you to some great resources by emailing info@studiobambooyoga.com.
For more information on the benefits of yoga and multiple sclerosis, this article by Victoria Swajcer, BSCPT, is available on the Can Do MS website, www.mscando.org.
Physical Therapist
Sue Kushner, MS, PT
Can Do MS Programs Consultant
Massage therapy can be a wonderful and useful tool in the “MS toolbox.” The benefits can range from relaxation, stretching of muscles, relief of “trigger points,” alleviating sore muscles, and helping with muscle imbalances. Due to the variety of symptoms that MS can cause, the benefits may vary from person to person.
Asymmetrical changes in the body may occur from tightness, weakness, sensory changes, or spasticity. In any of the cases, the resulting pain may be reduced with massage. Posture is often affected by these MS symptoms, which is another area that massage can prove to be beneficial. Soreness form overcompensation and/or use of assistive devices may also lead to musculoskeletal discomfort that can be lessened through massage.
As a massage therapist, my biggest advice would be to be careful of spasticity. Massage can provoke spasticity if not done properly. If the massage therapist knows MS and is familiar with spasticity, they will be able to gauge tight areas, amount of pressure to be used, and also know when an area should be avoided. The National MS Society has wonderful resources that can educate you on spasticity. With your MS clients, I would make sure to go easy for the first visit or two, and be cognizant of asking for feedback.
Here are some resources on massage and MS that may be helpful:
Registered Dietitian
Baldwin Sanders, RDN
Can Do MS Programs Consultant
Magnesium is a mighty mineral that is a co-factor in more than 300 enzyme systems that regulate biochemical reactions, such as protein synthesis, muscle and nerve function and blood pressure regulation. 50 to 60% of the body’s magnesium is present in the bones and contributes to structural development. Magnesium is widely distributed in plant and animal foods. Green leafy vegetables, beans, nuts, seeds, and whole grains are good sources. Magnesium is the primary ingredient in many remedies for acid indigestion (i.e. Rolaids) and laxatives (i.e. Milk of Magnesium). Therefore, you may run into problems if you consume too much magnesium.
Magnesium deficiency due to low dietary intake is rare. Deficiencies may result from some health conditions, chronic alcoholism, or the use of some medications such as diuretics. Gastrointestinal diseases such as Crohns, Celiac disease may lead to a deficiency due to malabsorption. Signs of a magnesium deficiency can be fatigue and weakness, numbness, muscle contractions and cramps, tingling, headaches and abnormal heart rhythms – symptoms that are also seen in neurological diseases like MS.
There is little research investigating magnesium and MS. There is one study that suggests magnesium oral therapy has “significant improvement” on spasticity in MS with no side effects. By addressing magnesium deficiencies, you may also see improvement in muscle spasms, weakness, twitching, muscle atrophy, incontinence, vision and hearing issues, osteoporosis, and epilepsies.
A good diet is the best way to consume magnesium. However, magnesium supplements are fairly well tolerated and safe, but will probably provide little relief to your MS symptoms. I would consult your doctor or dietitian before taking supplements. If they are suggested, beware magnesium supplements come in a variety of forms, including aspartate, citrate, lactate, chloride, oxide and sulfate. I would recommend the aspartate, citrate, lactate and chloride forms, as they are absorbed more completely and are more biodegradable than the oxide or sulfate forms. Magnesium supplements may also interact with some medications, and may reduce the absorption of biophosphonates, such as Fosamax, and antibiotics. Antibiotics should be taken 2 hours before or after magnesium supplements.
For more information on supplements, there are some great resources on the internet, including this brochure by the National MS Society. Thank you for submitting your question!
Physical Therapist
Sue Kushner, MS, PT
Can Do MS Programs Consultant
Exercise can have positive effects on lesion prevention because of “neuroplasticity,” the amazing ability of the body to form new neural connections through repetitive practice of physical and cognitive tasks. It is sometimes described as remapping and can show improvements in patients’ cognitive and physical functioning. One of the best articles that I like to reference, and that we often mention at Can Do MS, is by LJ White and V. Castellano in “Exercise and Brain Health-Implications for Brain Health-Part 1: Neural Growth Factors” in SPORTS MEDICINE, 2008, Vol 38, issue 2, pp. 91-100. It goes into detail about how exercise not only helps with the physical factors that we know (strength, cardiovascular fitness, etc.), but also assists with neuroprotection, neuroregeneration, neurogenesis and neuroplasticity. Therefore, quality of life can be enhanced. The article also touches on the effects of exercise on the inflammatory process. Another interesting article is by I. Lipp in FRONTIERS IN NEUROLOGY , 2105, Vol 6, pp 59-64. Titled “Neuroplasticity and Motor Rehab in MS.” Somewhat similar info, but mentions factors other than exercise.
Occupational Therapist’s Response
Ann Mullinix, OTR/L
Can Do MS Programs Consultant
Occupational therapy’s main goal is to keep people performing the activities that are important to them, modifying or adapting as needed. When fatigue is a roadblock, we instruct strategies to overcome the barriers, allowing more success and accomplishment. We all know how important exercise is for our overall health and wellness, and it is an important ingredient to also fight fatigue. Making exercise a priority is essential for fatigue management!
Neurologist’s Response
Barbara Giesser, MD
Can Do MS Programs Consultant
People living with multiple sclerosis who experience disease progression resulting in limited mobility are at risk for some complications. They include deconditioning, decreased cardiovascular function, bone loss (osteoporosis) and blood clots. Because of this, it is important for you to try to exercise as much as is possible.
For those individuals who cannot use their legs, you can participate in aerobic exercise with a hand cycle. Standing and weight bearing is also exercise, and for you since you cannot stand unaided, this may be accomplished with a standing frame. Stretching is also important to decrease spasticity, prevent contractures and maintain flexibility, and may be done with a helper, if you cannot do it independently.
Physical Therapist’s Response
Mandy Rohrig, PT
Can Do MS Programs Consultant
First, I would encourage you to get connected with a rehabilitation specialist (Physical Therapist or Occupational Therapist) who can help you prioritize exercises of greatest value, so that you are not exerting unnecessary energy on activities that are not providing you benefits to your overall function. With your therapist, I would encourage you to set realistic goals so you know what you are working towards and why you are working towards it. Having goals improves adherence to the exercise program, making it more likely for you to be successful!
Often it is thought that all exercise has to occur during 1 session. However, considering that fatigue is a significant issue for you, you may find it beneficial to complete smaller, incremental bouts of exercise intermittently throughout the day. For example, flexibility exercises with a support partner when it is convenient for him/her in the evenings and strengthening activities for the arms in the morning when you may be less fatigued. If you are unable to get to a gym and do require some assistance to effectively complete exercise, consider discussing with your health care team about resources that could come into your home to help with exercise. For example, a rehabilitation professional could instruct a college student or physical therapy student how to properly help you with exercises.
Since you use a power wheelchair for primary mobility, it becomes increasingly important to have a consistent flexibilityroutine. Prolonged sitting can exacerbate muscle tightness and spasticity. Consider referring to the National MS Society for a partner stretching manual; also, www.mymsyoga.com is a nice resource for adaptive yoga poses. Remember, these poses can be adapted even more for you in a seated or laying down position! I would also strongly encourage you to adapt a consistent aerobic exercise routine. Arm bikes or pedal exercisers can be purchased for around $30-$80 and can easily sit on a table. Strengthening activities for the arms can be completed with soup cans or elastic bands. Lastly, consider regular standing with assistance from walkers or standing frames. Regular standing is beneficial for muscle strength and flexibility as well as esteem. Consider the Multiple Sclerosis Association of America or National MS Society for assistance for funding of exercise equipment and discuss your needs with your health care team as insurance may help, too.
Physical Therapist Response
Susan Kushner, MS, PT
Can Do MS Programs Consultant
It is hard to assess exactly what is weak on this patient that is not allowing her to come to standing with ease. It could be any of the leg or trunk muscles, or balance, lack of range of motion, etc…
That being said, I would have a few suggestions:
-If possible, always walk with someone who would be able to help in case of a fall, or if she is alone, make sure she is in an area where someone could help her if she does fall.
-Use 2 forearm crutches, 2 canes, 2 walking sticks, or a walker when going for a walk. If she would fall, she can use the 2 points of support to help push herself up versus just the single cane. Or she may want to have a single cane, but carry one of the folding canes in a bag or purse so again, she’d have 2 bases of support to help herself up.
There is a great resource from the NMSS for both the patient and the PT. It is a binder that is an 8 week, once/week course that is titled “Free from Falls: A Comprehensive Fall Prevention Program for People with MS”. It is excellent.
Yoga Instructor and MSCS Physician Assistant Response
Amy Dix, MPA-C, MSCS
Can Do MS Programs Consultant
Thanks for this great question! My suggestion is to meet with a multiple sclerosis trained MSCS physical therapist to learn more about the disease presentation, as well as the disease in general to understand the primary weaknesses found in your students living with MS. When training local yoga instructors to teach MS patients, I require them to read MS for Dummies as well Dr. Randy Shapiro’s book titled Symptom Management in Multiple Sclerosis.
In general, when instructing students with MS, fewer poses is best, to encourage little to no heat. Also, using chairs with blocks under the feet for core strength is vital. Even if the student does not look like they have MS, they still experience invisible symptoms and their balance is affected by the MS. Encourage your students to do daily stretches, twists and anything to promote good bowel and bladder function. Don’t forget that in the beginning, yoga was one-on-one instruction, and often, that same individual attention is needed when you have MS. Iyengar and Jois had to “heal” and serve those living with chronic illnesses, and it is still often required to guide each pose daily to help those with MS.
Namaste!
Physical Therapist Response
Patricia Bobryk, PT
Can Do MS Programs Consultant
Being consistent with an exercise program is always a challenge. Many factors come into play:
time constraints, energy level, other obligations and even motivation. My best advice for
incorporating exercise into your daily routine (whether it is stretching or any other form of
exercise) is to follow the philosophy of intermittent exercise. If you can view your exercise
program as a series of short bouts of activity that you intersperse throughout your day, it
becomes much more manageable than trying to carve out 30 or 40 minutes out at one time.
Here are some examples of how you might incorporate stretching into your day:
• Do one or two of your stretches before you get out of bed in the morning (as long as you
can wait to use the restroom).
• Do one or two standing stretches every time you stand up or go to the kitchen for a
drink.
• While you are watching television, stretch in between each show during the commercial
break, or better yet, stretch during every commercial.
• Find the stretches that give you the most “bang for your buck” – the ones that address
the most problematic areas, and be sure you do those first. If you need help determining
which muscle groups need the most work, consult with a rehab specialist that has
knowledge of MS.
• When you are on the phone, a passenger in a car, at a movie theater, sitting at your
desk, standing at the sink to wash your hands, take a couple of extra minutes and
stretch!
A classic book on stretching is titled Stretching by Bob Anderson. This book provides hundreds
of stretches that you can do in any position and also has specific stretches for specific activities.
Although this book is not geared directly towards individuals with MS, it gives great suggestions
on a variety of stretches. Remember, to reap the greatest benefit from a stretch, you must hold
it at least a slow count of 30 seconds, repeat two to three times on each side and no bouncing
(this can cause micro-tears in the muscle).
Good Luck!
Occupational Therapist Response
Linda Walls, OTR
Can Do MS Programs Consultant
Stretching is an important part of helping us stay active, and though we often think we can not fit
one more thing into our busy lives, it is possible. To begin with, you have identified that
stretching makes you feel better, and you recognize it is important. This is the first step to
making it happen! Managing our time helps us manage our energy.
Managing our time can be organized into a few steps.
• First, Plan ahead, if activities are planned they are more likely to occur
• Second, Prioritize, if you feel something is important, you are more likely to find the time
• Third, Pace yourself, consider your day and choose those activities that can be
balanced between high and low energy tasks, for example while checking messages, sit
and stretch your ankles, or stretch your arm down your side several times.
To help you incorporate stretching into your daily routine, here are a few suggestions to help
prioritize stretching into your day:
1. Make a plan. Identify three to five stretches that you feel are most important. Try to
match these stretches to movements you are already doing. For example, while in the
shower, be sure that you are standing tall and pulling your shoulder blades back. Or,
when you are drying off after your shower, concentrate on stretching slowly up and down
each leg. Another example may be while at the bathroom sink brushing your hair or
brushing your teeth, try doing several arm reaches to the ceiling, or leg lifts to the side.
Another example would be when you are getting dressed, sit down and stretch your leg
out in front, to the side or add a few trunk twists. Though this may seem like adding time
to your morning routine, the stretching will allow your movements for the day to become
smoother, as you work out the stiffness in the mornings.
2. Another consideration in time management is to start simple. Identify a few stretches
that make your feel good. Adding three stretches to your morning routine should only take a few minutes. As you do these stretches every day, they will start blending and become part of your routine. Then as these stretches blend into your routine, you can add or switch stretches to address other muscles in your body that would benefit from daily stretching.
Hopefully, with these ideas you can find a starting point for yourself, and move into your daily stretching plan!
Occupational Therapist Response
Anna Cotton, OTR
Can Do MS Programs Consultant
This is a great question. I am sure that many people with MS have experienced stamina issues at one time or another. Have you talked with anyone else with MS on how they handle their stamina? I have found that some of the best solutions come from my patients sharing with one-another. I encourage you to see what those around you do to handle to the same issue, as it is very common.
To address stamina, or energy, we have to start with the building blocks: energy banking and energy spending. Some of the ways you can bank energy is through getting quality, un-interrupted sleep at night, taking rest breaks during the day and eating well—just as you said. The way you spend energy is on physical, mental and emotional tasks—ones that you have to do and ones that you want to do. Unfortunately, this simple equation of energy in and energy out can be disrupted and made highly variable due to MS. Therefore, you have to utilize strategies to manage your energy and think about it more than you may have had to pre-MS in order to have the stamina to get through the need-to activities and hopefully some want-to activities as well. Here are some strategies that may help.
Plan ahead: Know what is coming up in the hours and days ahead so that you can make conscious decisions about how to spend your energy and bank your energy. To do this, you can use a calendar to schedule “appointments” for afternoon naps, healthy snacks or a regular bedtime. Then, most importantly, follow the schedule to ensure you have enough stamina for what you’ve planned for. If you find yourself fatigued and not able to make it through a day as you planned, use that as an opportunity to reflect and make appropriate changes for the next day.
Prioritize: Examine your have-to list and want-to list. It sounds to me from your question that you’re missing out on some of the want-to activities in your life. These are important, too! Are there any have-to items that you can do in a different way (simplify, do less frequently, etc.), delegate to someone else in your family or hire someone to do to allow for more energy to spend on leisure or play activities?
Monitor: What takes the most energy out of you? Is your fatigue constant or does it vary? Does it become worse with heat? Are physical, mental or emotional activities most tiring? Only you can monitor what you feel like and what helps and doesn’t help. Try keeping a written log for a week to understand what triggers fatigue and what helps you recover. Play around with different strategies like using cooling devices, taking rest breaks, and breaking large tasks into smaller ones. Another strategy is altering activities throughout the day to use different types of energy – physical, mental and emotional. For example, if you finish paying your bills online and balancing your accounts, you may need to give your mind a break so choose a physical activity instead of another mental activity.
Be flexible: Above all, being flexible to the needs of your body and how it may change day to day is key. Accept that as much as you plan, prioritize and monitor your energy bank and expenditure, you may have days when you just can’t make it through. Also, be flexible to doing things in a new way. For example, using a motorized cart at the grocery store—even if you don’t have to for mobility reasons—so that once you arrive home, you have enough energy to put the groceries away and spend quality time with family/friends or doing an activity you enjoy.
I wish you the best and encourage you to share what you learn with those around you—I assure you it will be valuable to others!
Dietitian Answer
Baldwin Sanders, MS, RD, LDN
Can Do MS Programs Consultant
Thank you for your question. This is a common concern. Unfortunately, your caloric requirements are reduced with your MS due to limited exercise and fatigue. This makes weight loss more difficult but not impossible. It is important that you lose weight slowly and without fad diets, or it will come back. Your goal should be to lose no more than ½ pound per week. Make small steps, but be consistent.
For your fatigue, you want to reduce the size of your meals and include high protein snacks. Mozzarella cheese sticks, yogurt and cottage cheese with fruit are examples of smart snacks. It is important to engineer your environment. By that, I mean, make sure your home is conducive to your eating well. Stock it well with Lean Cuisine type meals, soups, fruits and vegetables, and get rid of high calorie snacks and sweets. Shrink your portion sizes, and load up on vegetables. For example, if you have a sandwich for lunch, save half of it for your afternoon snack. Eat baby carrots with it to fill you up and slow you down, so you will feel satisfied with less. I understand that eating at restaurants is tempting when you are fatigued, but this may double your caloric intake. When you prepare a meal or soup, make double so that you can freeze it and come home to a delicious meal when you don’t feel like cooking.
You can get a personalized eating plan from www.ChooseMyPlate.gov. You may want to consult with a registered dietitian. You can find a RD in your area through the website www.eatright.org. Good luck.
Physical Therapist
Michele Harrison, PT, ATRIC, ATP, CSMS
Can Do MS Programs Consultant
Your question brings up a lot of questions for me, as a physical therapist, trying to help someone living with MS learn how to exercise at appropriate levels while not increasing their symptoms of fatigue, weakness and imbalance. It would be very helpful to know what types of exercise you have tried. It would also be helpful to know the intensity levels and the length of time that you have tried to work out. It is a good idea to have a physical therapist or exercise specialist that is knowledgeable in MS and the variety of symptoms that are common for people with MS to assess your current strengths and areas that you need to work on. This would include assessment of your flexibility, muscle stiffness and range of movement, strength, balance, sensory issues, current mobility, exercise and activity levels. All this information helps a therapist individualize an exercise program specifically for your needs, current lifestyle and schedule. Participating in a graded exercise test will help give you the most specific information you will need on your current fitness levels and how to start a program from your current abilities. Good fitness is a combination of not only strength or aerobic exercise, but it also includes flexibility, coordination, balance and posture. Many people are good at one or a few of these components of fitness, but often people don’t incorporate all the areas. A therapist can help design a well rounded program of all of the needed components.
The types of activities that you choose to utilize for exercise may be the key to your success. For example, if you try to walk for increasing your endurance, but you are unable to do this for any length of time without great amounts of fatigue, then walking may not be your best idea for endurance training. Riding a stationary bike or a trial of water walking or deep water suspended activities may enable you to reach your goal of better cardiovascular fitness without the increase in fatigue. Another question to ask and address is if you experience heat sensitivity. If so, then utilizing or learning cooling techniques or use of a swimming pool that is the appropriate temperature for aquatic exercise may be key to your success in an exercise program.
I implement a lot of aquatic exercise into my treatment planning, and I run a number of aquatic exercise groups for people with MS. I find that the water is a supportive environment for people to exercise, walk and balance. The buoyancy, viscosity and hydrostatic pressure of the water often make people more independent and able to participate in higher level skills that they may not even attempt on land. The good news is that the work in the water has been shown to improve strength, endurance, flexibility and balance on land.
It may be that starting with 5-10 minutes of walking in the water (water about waist height) at a light to moderate pace is an adequate start to improve endurance and not trigger symptoms of fatigue. Adding just a few minutes to the time every week or so may be a good way to address the fatigue issue. You could also incorporate a 5-minute segment and then rest followed by another 5-minute segment. This may be an alternative way to decrease fatigue. Begin balance training by standing on one leg at a time at the edge of the pool, holding on if needed but trying to stand on one leg for 5-10 seconds. This may also be a starting place for improving balance.
There are as many variations to exercise programs, as there are people that want to exercise. You would find the most effective results by getting in touch with your local therapist or exercise specialist to help you create our plan.
Physical Therapist Response
Mandy Rohrig, PT, DPT
Can Do MS Programs Consultant
Thank you for your question, and I commend you on your efforts and diligence with an exercise program. Your question likely resonates with many people.
I would first recommend considering breaking up or sprinkling your aerobic exercise throughout the days you elect to do it. So, for example, if the goal is 15 minutes of aerobic exercise, then perhaps three, 5-minute sessions may be more manageable and less fatiguing. Another consideration would be incorporating the use of cooling products to maintain or decrease your core body temperature either before, during, and/or after exercise to improve tolerance. As little as 10 minutes has been shown to reduce fatigue secondary to heat sensitivity. There are many cooling products available, and I would recommend consulting the National MS Society or the MSAA for additional information on the cooling devices that exist. Lastly, I would encourage use of the Rating of Perceived Exertion (RPE) scale to monitor your intensity. This is a 0 to 10 scale, with 0 as no effort and 10 as extreme effort. Ideally, you should be exercising at a 3 to 4/10 intensity. Use this scale to help you better pace your workout.
Furthermore, I would also encourage you to consult with a physical therapist to help pinpoint precisely how to modify your exercise routine to maximize your energy.
I do hope this helps, and I wish you well on your exercise!
Registered Dietitian
Baldwin Sanders, RD
Can Do MS Programs Consultant
Thank you for the great question!
There is little evidence that “detoxing” eliminate toxins from your body. In fact, detoxing can “shock” our bodies (particularly if MS over-sensitizes your immune system) and can actually release more toxins. Any kind of stressor, whether it be emotional, mental, physical or environmental can have a negative impact on this illness. A sudden change of diet is no exception. This doesn’t mean you shouldn’t start including fresh juices into your diet. Juicing is a great way to get nutrients! When you drink juice, highly concentrated vitamins, minerals and enzymes rapidly enter the bloodstream absorbing all of the nutritional benefits of the fruits and vegetables and giving your digestive organs a much-needed rest. If you purchase a juicer or blender, it should supply recipes. There are also zillions of recipes online, including a couple of great “Juicing Recipes for Multiple Sclerosis” recipes found here: http://www.juicingrecipesforeverything.com/JUICINGRECIPESFORMULTIPLESCLEROSIS.html.
Can Do MS also hosts in-person workshops, where you can learn about juicing and another strategies for eating healthy with MS! Visit the Can Do MS website at www.mscando.org to learn about 1, 2, and 4- day programs coming to your area!
Please also read this great article on Healthy Eating and Multiple Sclerosis written by a fellow Can Do MS Programs Consultant, Aliza Ben-Zacharia, ANP, DNP, MS. http://www.mscando.org/living-with-multiple-sclerosis/can-do-library/ms-education/healthy-eating-multiple-sclerosis.
Physical Therapist Response
Patty Bobryk, MHS, PT, MSCS, ATP
Can Do MS Programs Consultant
Thank you for this great question!
As we begin the New Year many people are thinking about starting an exercise program. The many benefits of exercising include increased strength, increased flexibility, improved endurance and improved balance. All of these areas can help support your functional goals of
better walking, better stamina to perform your activities of daily living and to do things you enjoy.
There is no one exercise or type of exercise that is better than another in regards to MS. As the symptoms of this disease are very individualized, I always recommend being evaluated by a physical therapist to see what areas, if addressed, will give you the most benefit. When you have that information an exercise program can be tailored to your exact needs and goals. It is important to remember if you have limited energy, you want to get the most out of your exercises. Working on activities that are focused specifically on what you need will give you the most benefit.
The manner in which you do the exercise is as important as what type of exercise you do. The philosophy of intermittent exercises is a very important concept to follow. It has been shown that if you do exercise in shorter bouts without fatiguing yourself, all of the minutes of exercise add up and can actually allow you to do more than if you did one longer session a day. This concept keeps you from overdoing and prevents you from having a long recovery period after your exercise routine.
In regard to videos, I recommend that you try out a type of exercise video that interests you. You will be more apt to be consistent if you pick something that you enjoy doing. Yoga, tai chi, and seated workouts are just a couple of examples of types of exercise that may be appropriate for you. Many of these videos can be found for free on YouTube or other websites. Modify them as you need to (or ask your physical therapist to help you) and to stop before you over fatigue.
Enjoy and I wish you great success!
Physical Therapist Response
Susan Anacker, MSPT
Can Do MS Programs Consultant
Congratulations on showing your Can Do spirit and modifying your exercise world to fit your MS!
Yes, I agree that you should use your ankle brace when you use your exercise bike. The brace will help protect your foot and ankle, keeping them from slipping off the pedal and possibly getting injured by the spinning pedals. With the brace you will be able to bike further. Using an exercise bike will improve your cardiovascular health, strengthen your legs and fuel your “Can Do” optimism. I would suggest starting with frequent short sessions. (for example, 5 minutes 6 days per week is better than 30 minutes 1 day per week) Start with low resistance. Your goal is a brisk cadence with a free, light feel. The best indication of how hard to work is the perceived exertion scale. (my.clevelandclinic.org/heart/prevention/exercise/rpe.asp) This is a method to rate how you feel as you exercise, and use this feeling as a guide to exercise intensity. Generally you should strive to exercise in the moderate, 3-4 range on a 1-10 scale. Increase both time and resistance slowly. (For example, increase time 1 minute every 2 or 3 days). At the end of the session you should feel pleased with you accomplishment and eager to bike again tomorrow. Make sure to take a moment at the end of each workout to celebrate your accomplishment. This is the fuel that keeps all of us coming back to exercise again.
As you continue on your exercising adventure you may want to do some daydreaming about real life biking (with ankle brace, of course), trying one of the numerous biking options available these days. (Reclining bike, tandem bike, three wheel bike, cruiser bike, electric bike…assist when you need it, no assist when you feel fresh.)
Again, the goal for all of us is to modify our environment to allow us to exercise more and feel the joy of movement. Thanks for showing us the way! See you on the bike trail!
Here are a few links to information on biking for people with differing abilities.
www.dsusa.org/equipment-cycling-Providers.html
www.thebikerack.com
www.ilovebikes.com
Occupational Therapist Response
Linda Walls, OTR
Can Do MS Programs Consultant
There are several points to make in answering this question. First, exercise is good for someone who has MS, just like it should be a part of everyone’s regular routine. Your body benefits from exercise in that it keeps your muscles stretching and strong, exercise also gives you the benefits of a good cardiovascular system. If you used to use an exercise bike in the past, then finding a way to continue using it, is a good idea. Sometimes, in order to accommodate the changes in our body, we need to make modifications so that we can continue to exercise.
Second, to address the concerns with the ankle brace. The best answer would be to talk with the professional who provided you with the brace, to make sure there are no contraindications. If the brace is a simple device designed to help promote your ability to keep walking safely, then you can consider moving to the next step. If you decide to try using the bike with the brace on, make sure the brace fits well and does not irritate your skin anywhere. Each time you exercise with the brace on, check your skin afterwards and look for red irritated areas that do not fade within the hour. Also, begin with a short period of time, and slowly build. For example, exercise with the brace for 10 to 15 min. then check your skin. After successfully tolerating the 10 to 15 min. interval for several days and no skin irritation, increase the amount of time slowly, always checking your skin. This general idea of slowly increasing your tolerance for wearing a brace while exercising applies to many types of braces and supports.
Thirdly, when you begin to participate more in your exercise routine, take time to pay attention to how your body is responding to the increased exercising. Take time to allow your body to recover, and notice if the increased exercising impacts your overall level of fatigue. A regular exercise program should help you manage your energy levels and hopefully even provide your with an increased level of energy.
Question submitted by Kevin Walter, CAN DO Program Graduate, 2010
Exercise Physiologist’s Response
Alexander Ng, PhD
Can Do MS Programs Consultant
Kevin,
The nature of your question leads me to believe that you are initially referring to recovery from physical activity or exercise. Recovery is directly related to the activity that causes the physical fatigue. The more intense or harder the activity, and the longer the duration of activity, the longer will be the recovery time. If you are having difficulty recovering from exercise then try to cut back on either the exercise difficulty, duration, or both. If you wanted to maintain a certain moderate or perhaps high intensity then I would recommend breaking it up into smaller time blocks.
As mentioned in a previous question/answer the exercise does not have to be
continuous for you to receive a benefit. Proper nutrition is also important to
the recovery process. In addition, adequate nutritional support is necessary to maintain muscle mass and body weight… the second part of your question. If maintaining or increasing muscle mass and strength is a goal then I would make sure you are doing some appropriate strength or resistance exercise in addition to whatever aerobic exercise you may be doing. A YMCA would be a good place to start a formal strength training program as their personnel are usually pretty competent and can have experience with “special populations”.
Regardless, speak to an experienced exercise, rehabilitation, or related professional for proper strength training techniques and programs. In addition, there is also good evidence that strength training can help decrease symptomatic or “MS fatigue”, which you may have referred to as the last part of your question.
In short, pace yourself, eat well, and maybe add some strength exercise! I hope this helps. Good luck.
Nutritionist’s Response
Baldwin Sanders, MS, RD, LDN
Can Do MS Programs Consultant
Your diet can have a big influence on your fatigue level. Skipping meals or going too long without eating can exacerbate fatigue. A quick breakfast of cereal, banana and milk or yogurt and fruit are better than skipping breakfast.
Having snacks available is important so you don’t go too long without food. High protein snacks are good as they tend to make you more alert. Sweets tend to make you sleepier. Carrying mozzarella cheese sticks, a handful of nuts, or a container of yogurt can help you make it to supper.
A good idea is to have some frozen meals available so when you get home you have something quick and easy to microwave. Otherwise you tend to go with
anything that is there, chips and salsa, etc. When you are cooking something
good, cook in bulk and freeze for later. Make large batches of soup, and freeze
in individual servings so you have a quick fix for lunch or supper.
Occupational Therapist’s Response
Juliann Hanson-Zlatev, OTR
Can Do MS Programs Consultant
This is an excellent question, Kevin.
The first “trick” to managing physical fatigue is in utilizing 2 strategies to
your advantage. Pacing yourself and prioritizing your schedule and intensity of activities is paramount to achieving your goals and managing fatigue.
1) Pacing: To pace yourself effectively you must strive for a
fairly consistent level of physical activity each day. It is helpful to think
of the whole of your day in order to do this, including mundane/everyday chores
because everything you do requires your energy. For example: Avoid working
very hard for 1-2 days then “resting” or “collapsing” for several days because
you will have depleted your resources and your body will have difficulty in
anticipating your needs. This also applies to the intensity of your workout as
well. The more consistent your work out is the better your body will maintain
muscle mass and skill. The more consistent you are the more your body and mind
“absorbs” the skill and you will use less energy to perform it as time goes on.
(Another example: an Olympic skier exerts less energy skiing bumps than the
rest of us; mundane activities use less of our energy than when we are learning
a new skill).
That said, there are always exceptions and you may wish to plan ahead with your
schedule to anticipate a long or challenging day by planning into subsequent
days your rest breaks. For example: you may wish to go out with friends or
family one evening; the following day you may want to plan a lighter day so you
will not use as much energy. However, you would still plan activities for the
following day – just lighter.
2) Prioritizing: This helps you get the chores/activities that are important to
you done. When we fail to prioritize we set ourselves up for disappointment or
overdoing it just to accomplish our list! Placing high priority tasks/chores at a time of day that ensure they will get done helps us do just that – accomplish
our “’to do” list. Here is the great news: your priorities can shift and
change and do not have to include only work chores. Exercise, hobbies, friends and interests should also move into the #1 and #2 spot to balance and round out your life. Keeping exercise close to the top of your priority list will ensure that you build endurance, maintain body mass and skill level, and improve your cardiac capacity for improved longevity (read: less fatigue).
A final word on fatigue management; try to use as little energy as possible to
complete a given task. For example: sitting to perform any activity requires
less energy than standing to perform the same activity; so sitting to shave,
brush your teeth, prepare food, etc.can save muscle exertion and thereby grant
you more energy elsewhere in your day where you WANT to use it. Thank you for
asking an important question.
Question submitted by Dennis, CAN DO Program Graduate, 2009
Urologist’s Response
Susan Kolata, MD
Can Do MS Programs Consultant
There is no specific amount of water needed daily. In Arizona in the summer you
might need to drink 20 glasses of water to maintain a reasonable output if you
exercise in the sun. The more important question is how much urine output is
needed and what it takes to get there. If you produce stones, a reasonable
preventative output is 2 liters of urine daily. If you just want a minimal
output, it is one liter. In between would be best.
Many foods will help towards this goal as well, fruits, soups, vegetables, etc. Only high protein shakes/or bars, etc will take away fluids, but some drinks are
less desirable such as coffee, sodas and alcohol. Using bottled water can be
helpful in counting the volume -ie try and drink 1 bottle per 1-2 hours, or so
many per day – for those goal oriented people. Adding lemon juice or orange
juice to the water, making ice tea, finding a water, or water temperature that
is enjoyable, can be helpful. The ultimate goal is to produce urine that is
lighter in coloration (less concentrated), so stones are flushed out, bacteria
is flushed out as well as routine toxins.
Nutritionist’s Response
Denise Nowack, RD
Can Do MS Programs Consultant
Water is an essential part of your body’s daily routine. It helps in the digestion and transports other nutrients, controls body temperature and is important for brain function. It’s something we can’t live without.
It might be tempting to avoid beverages as a strategy to “manage” bladder problems. However, this can lead to dry mouth, loss of appetite, swallowing difficulties, headaches, constipation, deficiencies in certain nutrients, and increased risk for urinary tract infection.
Don’t despair if you don’t like water. It’s really about getting adequate fluids, and that can come from a variety of sources.
Here are a few tips to staying well hydrated:
* Start with your oral medications. Make it a habit to drink a full glass of water or juice each time you take your pills.
* Include other beverages at meal and snack time like juice, milk or sparkling
water. You can even make your own fruit spritzer by diluting your favorite fruit juice with sparkling water.
* Build in “water breaks” throughout your day.
* Pass a water fountain…take a drink.
* Carry your own personal water supply when you are out and about.
If you’re prone to urinary tract infections, include cranberry juice (or tablets). In addition to providing fluids, cranberry juice can be of added benefit in preventing urinary tract infections by preventing bacteria from sticking to the cells that line the urinary tract.
In addition to beverages, the foods you eat can help satisfy your body’s thirst. In fact, about 20% of our daily water intake comes from food, with fruits and vegetables having some of the highest water content (upwards of 80%) . Topping the list of juicy fruits and vegetables are lettuce, squash and watermelon (95%), tomatoes and broccoli (92%) and strawberries and peaches (90%).
A common serving of the following foods contributes about 8 ounces of fluids:
* Spaghetti with meat sauce
* Oatmeal with blueberries
* Chicken noodle soup
* Low fat cottage cheese with pineapple
Soups and foods with broth or cereals with milk are other great options.
Hopefully with these ideas you might find it easier than you thought to fit in
fluids into your daily routine.
Good eating!
Question submitted by Kay Roberts, CAN DO Program Graduate, 2001
Physical Therapist’s Response
Susan Kushner, MS, PT
Can Do MS Programs Consultant
Without knowing what the ankle problem is (weakness, bracing, etc) and whether you use an assistive device, I would suggest that you ask each physical therapist WHY they are recommending what they are recommending. Most likely they each have good rationale behind their decisions and advice to you. It is up to you to use logic and maybe even practice as to WHICH suggestions will be best for your case, as long as you feel that nothing detrimental will be done to the ankle or put you in harm’s way, such as risking a fall. Feel free to gently say to one what the other one suggested and ask why the advice may be different. They both may have very good, valid points and a compromise may work.
Without knowing the specifics, I hope these suggestions help you.
Question submitted by Denise., CAN DO Program Graduate
Registered Dietitian’s Response
Denise Nowack, RD
Can Do MS Programs Consultant
Eating well doesn’t have to take a bite into your budget. A little work up front can save you time and money down the road. Here are some tips to keep a few pennies in your pocket without compromising your health.
Have a plan.
Look for healthy recipe ideas using budget-conscious ingredients. (Search the internet using the ingredient as the key word.) Create a master shopping list to keep your refrigerator and pantry filled with staples that are quick and easy to cook, and kind to your wallet. These can include:
* Pastas
* Quick-cooking grains (like quinoa, couscous, brown rice)
* Canned beans (a great source of fiber and protein)
* Soups (choose reduced-sodium varieties)
* Canned & frozen fish
* Canned & frozen varieties of fruits and vegetables
* Nonfat powdered milk (use when milk is needed as an ingredient in cooking)
Shop smart.
* Clip coupons…or go online to look for discounts on the products you use most.
* Check your list and stick to it! Resist the urge to pick up “extra” items from end-of-aisle displays or at the checkout counter.
* Buy in bulk and store in ready-to-use portions. If storage space is limited consider splitting packages with a friend to take advantage of volume savings.
* Look for specials. Stock up on staples when they go on sale.
* Take advantage of fresh fruits and vegetables in season. For other produce, frozen and canned products can be good choices and just as nutritious as fresh. Opt for low-salt products and avoid those prepared in sauces or with added sugar.
* Go generic. Buying the store’s brand of canned, frozen or bagged foods can provide great savings without compromising nutritional value.
Make the most out of meals.
When you have the energy to cook, double up on recipes! Freeze the extra in oven-ready containers, or use later in the week for lunches or quick dinners. Leftovers from a roasted chicken at dinner can be reinvented the next night in as chicken pesto pasta or for lunch in a chicken salad. Leftover vegetables can give canned soups, rice or pasta a nutritional boost.
While pre-cleaned and precut produce can save time and energy in the kitchen they can be more expensive than their standard counterparts. Go for whole fruits and vegetables and cut them up yourself. Chop and package them in common portion sizes for the recipes you use most, or slice and store them for an easy snack.
Be a savvy snacker.
Healthy snacking can be your best friend in managing fatigue. However, single-serving snack foods can be costly. Create your own individuals snack packs. Make them in advance and package in individual snack bags so you can “grab & go.”
Physical Therapist Response
Kit Concilus PT, MS, OCS
Can Do MS Programs Consultant
I am glad to hear that you are still walking your dog. You are right about exercise being very important for you.
It sounds like it would be helpful for you to analyze what specifically is making the activity of walking the dog more difficult for you. It may be that you are experiencing problems with balance, endurance, coordination, fatigue, spasticity, muscle weakness, muscle tightness, joint stiffness, or some combination of these things. You can talk in detail with your doctor to help figure out which is affecting your dog walking the most, and come up with a plan to improve the situation. Sometimes subtle improvement in one of these areas can make a big difference in function. Maybe medication, exercise, bracing or other options can help you meet your goal. You can discuss the possibility of working with a physiatrist (doctor who specializes in rehabilitation) too.
My guess is that you could benefit from working with a physical therapist who is familiar with Multiple Sclerosis at this point. Therapists love to work with people who come to them with a clear, measurable goal such as “I want to be able to walk my dog for (so many) minutes.” Your physician can help you find the physical therapist. The therapist can measure your walking speed, take a close look at your musculoskeletal status and walking pattern, and develop a home exercise program that will help improve your ability to walk your dog, and fit into your lifestyle. During this process, remember to focus on what you CAN do. Happy dog walking!
Question submitted by Dan Melfi, 2011 CAN DO Program Graduate
Nutritionist’s Response
Baldwin Sanders, MS, LD, RDN
Can Do MS Programs Consultant
Vitamin D is a fat soluble vitamin most famous for its role, along with calcium, in bone density. It is actually a hormone because it can be manufactured in the skin, with the exposure to sunlight. Whether you receive your vitamin D from sun or food, it must be activated by the liver and then the kidney to function. The active form of vitamin D is Calcitriol. We obtain 80 to 100% of our vitamin D from sun exposure. The amount of sun needed depends on skin color, age, season, location and time of day. Generally, 15 minutes of sun exposure to hands, face and arms is adequate to synthesize the vitamin D precursor that is required. Seniors and those with dark skin need about 5 times as much. Other things that may affect your ability to absorb sunlight are pollution, geographic latitude, cloud cover, window glass, intestinal and kidney disease. There are few dietary sources of vitamin D. In the US, we fortify milk with 400 IU per quart by law, so all dairy products are good sources. Fatty fish are another good source. The Recommended Dietary Allowances for calcium have recently been increased to 600 IU for ages 1 – 70 years, and 800 IU for those over 70 years. One cup of milk contains 400 IU. Meeting the vitamin D RDAs may be difficult for people with lactose intolerance.
The main function of vitamin D is to maintain a normal calcium range and prevent rickets and osteoporosis. More recently, vitamin D is being studied as an important immune modulator in Multiple sclerosis. Low vitamin D levels are associated with a higher risk for MS. The geographic distribution of MS adds evidence as areas with more sunlight have a lower incidence of MS. Many physicians with MS clients are monitoring their blood levels of vitamin D and prescribing supplements. Please note: Blood levels should be monitored, and people should not dose themselves with Vitamin D without a physician’s supervision.
Neurologist’s Response
Barbara Giesser, MD
Can Do MS Programs Consultant
Vitamin D is gaining increasing recognition as an agent that has immuno modulating and anti-inflammatory effects. There are studies that indicate that sun exposure and Vitamin D levels early in life may influence a person’s risk of getting MS, i.e. less sun and lower Vitamin D levels are correlated with increased risk. For persons who already have MS, there is data that suggests that lower Vitamin D levels may increase the chance of an exacerbation.
Physical Therapist Response
Jane L. Wetzel PT, PhD
Can Do MS Programs Consultant
Exercise may improve all types of gait dysfunction in persons with MS.1 Muscles must be strengthened according to the amount of force they are able to produce. Aggressive exercise may actually make some muscles weaker. Resistive exercise for muscles that are graded 4/5 (60% of Normal) or 5/5 will actually help reduce overall fatigue and help your body compensate for those muscles that are unable to work against gravity (2/5 [10% of Normal] or less). However, if muscles are very weak (3/5 [20-30% of Normal] or less) orthoses are important to help protect the weak muscle and prevent overuse – especially during periods of exacerbation. Overworking weak muscles with exercise or ambulation without a leg brace may make the muscle weaker. Assistive devices and balance training may reduce gait dysfunction from imbalance.
Electrical stimulation may be used as a method of strengthening weak muscles. An investigation on the effect of 8 weeks of surface Functional Electrical Stimulation (FES) training to the quadriceps on the levels of general, central, and peripheral fatigue in MS patients revealed that general fatigue, central and peripheral fatigue and impact of fatigue significantly improved [Fatigue Index: FI (p = 0.01), Central Fatigue Index:CFI (p = 0.02), and Modified Fatigue Impact Scale:MFIS (p = 0.02)] after FES training.2 In this study it is likely that increasing strength helped improve the stronger muscles and decreased the amount of total contraction time of muscles during gait. Less contraction time happens when you move more efficiently and this means there is less chance for fatigue.
You can use electrical stimulation while moving light resistance to assist in strengthening your muscles for 3/5 muscles. However, long-term resistance training with electrical stimulation is no better than traditional strength training for improving function.3 One study recently demonstrated an improvement in EDSS score. Individuals with MS in this study had on average an EDSS score of 5.9 (range, 4.5-6.5). They received electrical stimulation for 140 days (range, 22-495). Mean EDSS scores improved by 0.78 (range, 0-2.0).4
Electrical stimulation may also be used as an orthotic in gait. There is evidence that walking with an FES stimulator may actually strengthen central nervous system connections as well as assist in the activation of weak muscles.5 Walking speed increased with the stimulator off (therapeutic effect) by 24% (P = .008) and 7% (P = .014) in the non-progressive and progressive groups, respectively. So it appears that individuals with non-progressive neurological conditions (like stroke) will receive a greater benefit in terms of improving central nervous system connections than people with MS who have a progressive condition. Another study examined patients with secondary progressive MS placed in one of two groups (home exercise vs. electrical stimulation). Those individuals who were given the home exercise program had significant improvements in their walking speed over 10 meters and distance walked in 3 minutes than those using FES training. Those with FES training did not have a significant improvement after 18 weeks of exercise6 when walking was tested without the stimulator in use.
However, the group using FES as an orthotic walked much faster with the FES than without the FES. So there is clearly a functional benefit. However, once the orthotic is off (walking to the bathroom at night) the PT guided exercise program offered greater improvement. There are many times when someone with MS and foot drop may need to move around without the stimulator.
What can you do with all this research??? Find a good physical therapist who has good knowledge of MS and who has examined your muscle strength in detail. If electrical stimulation is able to assist in clearing your foot during gait then it may be a wonderful tool to help you walk better. If your MS is involving your hip and knee flexion you may not find as much benefit from electrical stimulation designed to assist foot drop (common peroneal n. stimulation). Consider working on strengthening all muscles that are 4/5 or better in your hip and knee. This may reduce your fatigue. Be sure to work with your therapist so you know which muscles to try to strengthen and which muscles should really be protected (especially during an exacerbation). Sometimes a solid or articulating ankle brace may be a good way to protect your ankle muscles and keep you from overworking weak muscles. It may also allow you to safely clear your foot. Pay attention to all your symptoms whenever you try a new brace or a new exercise. If the new exercise makes you weak then let your therapist know. Exercises will need to be modified several times before the right strengthening program is achieved.
References:
Physical Therapist Response
Steve Molloy, PT
Can Do MS Programs Consultant
When it comes to juggling the demands of your personal life and career, finding the best way to include exercise in the equation can be quite a challenge. Throw the MS wildcard into the mix, and your equation is even more complicated. Unfortunately, there is no single exercise routine or schedule that is right for every person. The right exercise schedule for you is the one that works for you right now.
With this being said, I advise you to consult your physician and other health care providers to see if they have any specific concerns or precautions for you before you begin any exercise routine. Assuming they give you the all clear, my advice is listed below.
If you are just getting started, my advice is to start small and celebrate your success. Pick something you can do safely and easily, and then commit a small period of time to perform the activity several times a week. You get the biggest benefit in fitness when you change from doing nothing to doing something. You may start with 3-5 minutes of something easy, but the key thing is to get started. Remember you are exercising for you, and 3-5 minutes is more than 0 minutes from last week.
It may take some experimentation to hit the right combination of activities, frequency, intensity and duration that best supports your mission to lead a healthy, balanced life. I like to think of your exercise routine as a tool you will use to help keep your systems moving in the right direction.

I provide some concrete recommendations that apply to anyone designing or modifying an exercise routine:
Fun
If you are anything like me, motivation lags when exercise is a chore. Pick something that is enjoyable. Are there any exercise activities that you like doing? Are there any exercise groups you might like to be a part of?
Feasible
If the exercise activities you select are too much of a project, the odds of them ever becoming part of a routine are slim. Look for activities that don’t require you to move heaven and earth to make them happen. You are better off with simple exercises you can actually do.
When you are selecting an activity you should consider the following:
Frequent
Sporadic exercise is not an effective way to improve your conditioning. Hit and miss exercise sessions increase your risk of injury and won’t provide you with the gains you are looking for.
Fatigue Friendly
Remember, you are exercising to improve your health and well-being. Listen to your body and don’t go beyond your limits. Nothing is gained if your great workout wipes you out of life for the rest of the day!
Responses are provided as general educational resources and should not be interpreted as diagnoses, prognoses, or treatment suggestions.
More FAQs