Author
Roz Kalb , Psychologist
Close

1 Jun 2023 | ~5:06 Engagement Time
Changes in bowel function are common in MS – with the most common being constipation. When the nerve signals that provide communication between the brain and the bowel are damaged, the passage of stool can be slowed. The longer that stool remains in the bowel, the more moisture it loses and the drier and harder it becomes.
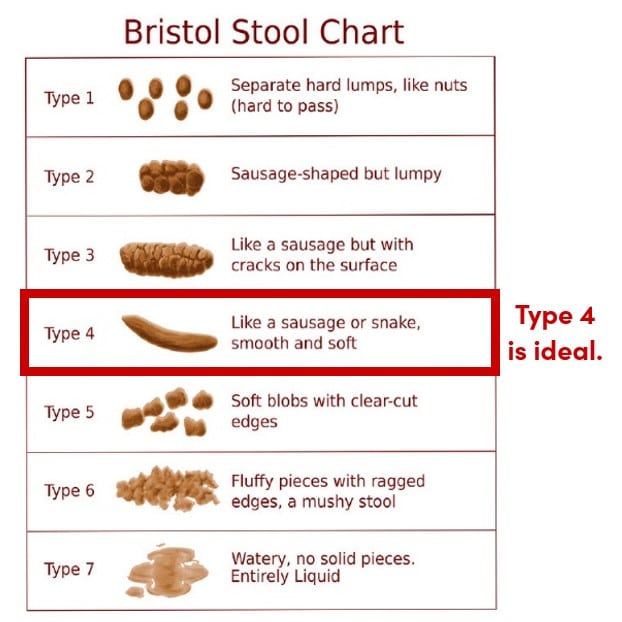
Constipation is generally described as having fewer than three bowel movements a week, with stool that is hard, dry, and difficult or painful to pass. The following chart shows examples of stool that range from hard and dry to watery. Type 4 stool is the type that you want to be aiming for because it is soft, smooth, and easy to pass.
Your food and drink choices have a significant impact on your bowel function.
When you move, your bowels move.
Your body gets used to certain rhythms.
If you notice changes in your bowel function that last more than a couple of weeks, discuss it with your MS provider.
It may occasionally be necessary for you to use a laxative to help with bowel movements.
The key to managing constipation is to proactively avoid it when you can with fiber, fluids, and physical activity, and to consult with your healthcare provider promptly if you need more help.
Keep Learning